With veterans at generally higher risk of lung cancer for a variety of reasons, the VA is seeking to catch cases earlier by instituting widespread screening. The healthcare system is facing a difficult challenge, however: A sizable percentage of veterans whose scans showed potential problems in a demonstration project never come back for follow-up screening and treatment. Here’s how the VA is trying to remedy the situation.
DURHAM, NC—Veterans have a higher rate of lung cancer and a lower rate of survival than their civilian counterparts, making early detection and prompt treatment a high priority for VA physicians. Early, regular screening is one way of helping clinicians identify at-risk veterans before it’s too late. However, like many preventive healthcare measures, compliance can be a challenge, and having a screening system in place does not always mean it will be used to peak effectiveness.
According to the national Centers for Disease Control and Prevention, lung cancer is the second most commonly diagnosed cancer in both men and women in the United States. Prognosis after diagnosis is poor, with about 90% of cases leading to death. Studies have found that veterans are 76% more likely to be diagnosed with lung cancer than those who did not serve in the military. One reason is that there is a higher prevalence in the veteran community. Another is exposure to toxic substances during their service, such as Agent Orange, asbestos, chemical weapons, and burn pits. Due to a greater frequency of comorbid conditions among veterans, their health tends to be poorer than the general population; consequently, they have a lower survival rate following a lung cancer diagnosis.
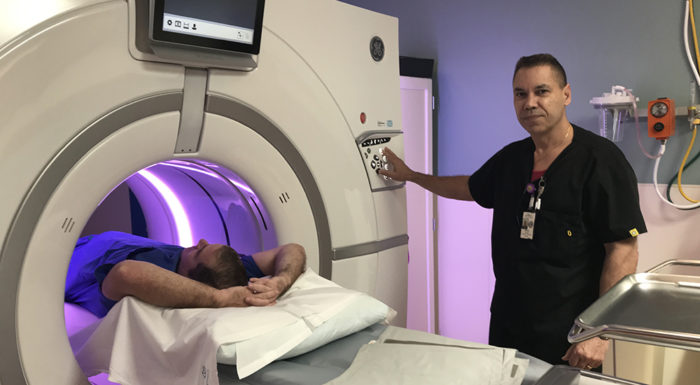
Early identification of lung cancer can lead to more effective treatment. Research has shown that lung cancer screening using Low-Dose Computed Tomography can help make that identification possible.
The National Lung Screening Trial—a landmark study whose results were released in 2011—found that a CT scan was more effective than the standard chest X-ray in detecting cancer and precancerous signs. Deaths in the CT scan group were 20.3% lower than the X-ray group. That trial resulted in recommendations by the U.S. Preventive Services Task Force in 2013 for annual lung cancer screenings using a CT scan for current and former heavy smokers.1
VA brought its own recommendations in line with the task force’s, recommending yearly screenings for patients 55-80 years old, who are current smokers or former smokers who quit less than 15 years ago and have a history of smoking at least the equivalent of one pack a day for 30 years.
With an eye toward a national screening program, VA embarked on a demonstration project to examine its effectiveness. In a study of 2,106 veterans across eight VA hospitals, screenings found that 56.2% had nodules that required tracking, 3.5% had possible lung cancer and needed further evaluation, and 1.5% had lung cancer. 40.7% showed other findings, such as emphysema, pulmonary abnormalities, and coronary artery calcification. Twenty of the 31 patients found with lung cancer were in Stage I, which meant effective treatment was available and that screening had a definite benefit.
The project also found that an effective screening program would come with challenges, including identifying veterans who would best be served by screening (pack years is not something regularly calculated) and getting initial buy-in from veterans. Only about 58% of candidates initially approached for the demonstration project agreed to be screened.
Follow-Up Screening
A follow-up study of that first demonstration project has added another challenge to that list—getting veterans to come in for follow-up screenings, especially if their first screening was negative.
The study conducted by the Thoracic Oncology Research Group at the Medical University of South Carolina in Charleston, was aimed at examining adherence to annual screenings following a baseline scan. Adherence was defined by the National Lung Cancer Screening Trial as having a follow-up LDCT within 15 months after the first scan. 2
Of the 2,106 veterans in the study, 60% had scans negative for nodules greater than or equal to 4 mm in size and repeated annual LDCT was recommended. In this group, 149 were considered no longer eligible for screening for a variety of reasons. Of the 1,120 remaining, only 880 went on to undergo a follow-up scan–a 77.6% adherence rate.
“Our study demonstrates that even within the context of a well-designed, implemented and guideline-adherent LDCT screening program, adherence is not optimal and does not reach the reported 95% [goal] of the National Lung Screening Trial when the baseline scan is negative,” said lead researcher Paul Brasher, MD. “Both mortality benefit and cost-efficacy are likely to suffer without better adherence.”
Since that initial demonstration project, VA has been developing ways to assist clinicians in identifying who needs to be screened, initiating conversations with patients about the benefits of screening, and making sure those patients return for follow-up scans.
“VA has developed several electronic lung cancer screening and lung nodule tracking systems to ensure that veterans receive screenings and appropriate follow-up,” explained Jane Kim, MD, MPH, VA’s chief consultant for preventive medicine, based in Durham, NC. “One system, developed by a team from VISN 23, has been disseminated to 16 sites across the organization with plans to implement in at least five more sites in 2019.”
“VA facilities that use an electronic lung cancer screening tracking tool can follow up with veterans to ensure that they receive recommended follow-up at the time it is due. Some VA facilities have lung cancer screening coordinators that reach out to veterans about screening tests,” Kim said. “In addition, there is a set of electronic decision support tools available for use in the VA medical record that prompts clinicians to offer and order lung cancer screening tests when recommended.”
Those electronic support tools include the Should I Screen online tool, which was accessed more than 270,000 times between January 2015 and November 2018. The tool helps patients and healthcare providers weigh the risks and benefits of lung cancer screening.
In 2018, VA researchers completed another tool specifically for clinicians—Lung Decision Precision.
The tool provides patient-centered recommendations based on individual risk profiles. It also offers evidence-based, personalized methods of discussing the benefits and harms of the test; allows clinicians to document their shared decision-making in electronic medical record systems; and enables them to share a printable report with patients.
“VA has developed a toolkit of materials to support lung cancer screening in VA medical centers,” Kim said. “This toolkit includes information on the VISN 23 tracking system and contains downloadable education materials for use by clinicians when having discussions about lung cancer screening with patients. It’s assisted a number of VA facilities in planning and implementing lung cancer screening programs for veterans who meet criteria.”
1 National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks JD. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011 Aug 4;365(5):395-409. doi: 10.1056/NEJMoa1102873. Epub 2011 Jun 29. PubMed PMID: 21714641; PubMed Central PMCID: PMC4356534.
2 Brasher P, Tanner N, Yeaker D, Silvestri G. Adherence to Annual Lung Cancer Screening Within the Veterans Health Administration Lung Cancer Screening Demonstration Project. Presented at CHEST Annual Meeting 2018. October 6-10. San Antonio, Texas.
Expanded Use of PET Increasing VA Small Cell Lung Cancer Survival Rates
DURHAM, NC—The VA is doing a better job in using imaging tools to stage small cell lung cancer, and the result is better survival rates.
That’s according to a new study published earlier this year in the Journal of the National Comprehensive Cancer Network.1
A study team led by researchers from Durham, NC, VAMC and Duke University pointed out, “Accurate staging for small cell lung cancer (SCLC) is critical for determining appropriate therapy. The clinical impact of increasing PET adoption and stage migration is well described in non-small cell lung cancer but not in SCLC.”
Their study sought to evaluate trends in positron emission tomography staging and survival over time in the VA Central Cancer Registry, as well as the effect of PET on outcomes.
To do that, researchers identified patients diagnosed with SCLC from 2001 to 2010, assessing PET staging, overall survival and lung cancer-specific survival assessed over time. The impact of PET staging on OS and LCSS was assessed for both limited-stage and extensive-stage SCLC.
Overall, the study team found, PET use in a total of 10,135 patients with SCLC increased from 1.1% to 39.2% from 2001 to 2010.
At the same time, the study reported that median OS improved:
- For all patients—from 6.2 to 7.9 months;
- Those with LS-SCLC—from 10.9 to 13.2 months; and
- Those with ES-SCLC—from 5.0 to 7.0 months.
Researchers noted that the proportion of ES-SCLC increased among staged patients from 63.9% to 65.7%. Among 1,536 patients with LS-SCLC treated with concurrent chemoradiotherapy, meanwhile, 397 were staged by PET. In those patients, PET was associated with longer OS (median, 19.8 vs. 14.3 months; hazard ratio [HR], 0.78; 95% CI, 0.68-0.90; P<.0001) and LCSS (median, 22.9 vs. 16.7 months; HR, 0.74; 95% CI, 0.63-0.87; P<.0001) with multivariate adjustment and propensity-matching.
In the 6,143 patients with ES-SCLC, PET was also associated with improved OS and LCSS, the according to the article.
“From 2001 to 2010, PET staging increased in this large cohort, with a corresponding relative increase in ES-SCLC,” the study authors concluded. “PET was associated with greater OS and LCSS for LS-SCLC and ES-SCLC, likely reflecting stage migration and stage-appropriate therapy. These findings emphasize the importance of PET in SCLC and support its routine use.”
1 Hong JC, Boyer MJ, Spiegel DY, Williams CD, Tong BC, Shofer SL, Moravan MJ, Kelley MJ, Salama JK. Increasing PET Use in Small Cell Lung Cancer: Survival Improvement and Stage Migration in the VA Central Cancer Registry. J Natl Compr Canc Netw. 2019 Feb;17(2):127-139. doi: 10.6004/jnccn.2018.7090. PubMed PMID: 30787126.
