ST. LOUIS – Medicare Part D could save more than $14 billion annually if it paid the same prices for top medications as the VA, according to a new study.
A research letter published earlier this year in JAMA Internal Medicine noted that some state and federal initiatives to reduce prescription drug costs have proposed using the VA as a model. That agency is known for its ability to obtain deep discounts on medications through direct negotiation with pharmaceutical manufacturers and the use of a national formulary, according to researchers from the VA St. Louis Health Care System and colleagues.1
The authors cited 10-year-old studies estimating that Medicare Part D could save $14 billion to $22 billion annually if it paid prices similar to those paid by the VA, as well as a recent congressional report4 for 20 brand-name drugs estimating potential annual savings of $2 billion.
The study team sought to come up with a better estimate, however, noting that none of those calculations used actual prices paid by the VA, which can be lower than published federal prices. To achieve that, researchers used the most recent national data available from Medicare and the VA “to quantify the savings Medicare Part D would achieve if it paid the same prices for prescription drugs currently paid by the VA.”
“Several state and federal efforts to reduce prescription drug costs have proposed using the Department of Veterans Affairs (VA) as a model, given its ability to obtain deep discounts on medications through direct negotiation with pharmaceutical manufacturers and the use of a national formulary,” the authors wrote “We used the most recent national data available from Medicare and the VA to quantify the savings Medicare Part D would achieve if it paid the same prices for prescription drugs currently paid by the VA.”
The review was performed with data from Jan. 1, 2011, to Dec. 31, 2016. In an effort to make Medicare and VA prescription spending comparable, the team used the database of all prescriptions dispensed by the VA from 2011 to 2016 and identified all matches for the Medicare medications, deriving comparable data on acquisition costs and quantity dispensed using the actual price paid by the VA.
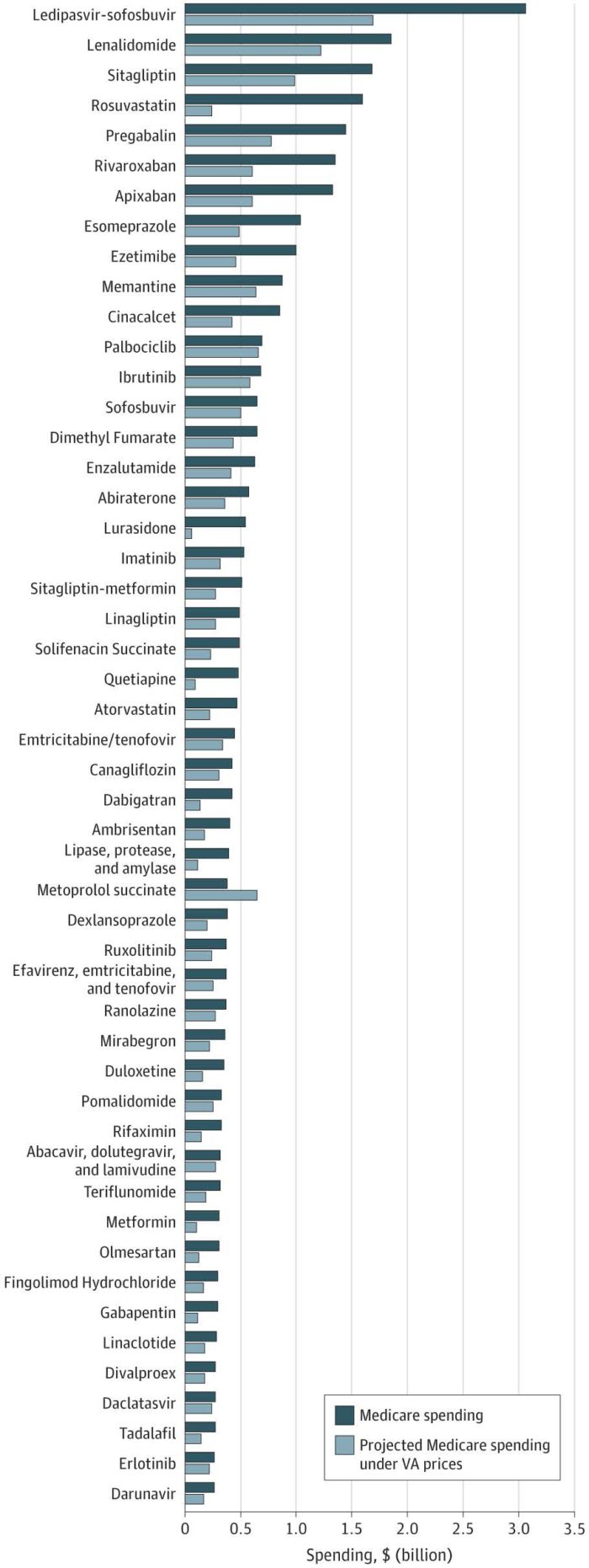
The study determined that the annual net Medicare Part D spending on the top 50 oral drugs ranged from $26.3 billion in 2011 to $32.5 billion in 2016. If Medicare Part D had obtained VA prices, however, the cost of the medications would have been $18.0 billion — a savings of $14.4 billion or an estimated 44%.
The research letter added that the projected magnitude of estimated annual savings from 2011 to 2015 was similar, ranging from 38% to 50%.
“To our knowledge, this is the most up-to-date analysis that directly compares prices between Medicare Part D and the VA, accounting for estimated rebates and using actual VA prices as opposed to publicly reported federal supply schedule prices,” study authors wrote. “Using these data, we calculated $14.4 billion in potential savings in 2016 for only 50 drugs.”
The issue is likely to be raised in the 2020 presidential campaign. Sen. Bernie Sanders,(D-VT), noted on his campaign website, “Under current law, the Secretary of the Department of Health and Human Services (HHS) is prohibited from negotiating lower drug prices on behalf of Medicare Part D beneficiaries. In contrast, other government programs, like Medicaid and VA, are allowed to negotiate. As a result, Medicare Part D pays on average 73% more than Medicaid and 80% more than VA for brand name drugs. The federal government could save between $15.2 and $16 billion a year if Medicare Part D paid the same prices as Medicaid or VA.”
In January, Rep. Peter Welch (D-VT) introduced in the House of Representatives the Medicare Prescription Drug Price Negotiation Act of 2019.
1. Venker B, Stephenson KB, Gellad WF. Assessment of Spending in Medicare Part D If Medication Prices From the Department of Veterans Affairs Were Used. JAMA Intern Med. 2019 Jan 14. doi: 10.1001/jamainternmed.2018.5874. [Epub ahead of print] PubMed PMID: 30640367; PubMed Central PMCID: PMC6439699.