By Brenda L. Mooney
PITTSBURGH—Is it better to use sodium bicarbonate or -N-acetylcysteine to prevent acute kidney failure related to common angiography procedures?
A new international study led by a VA came up with a surprising result: Neither of the agents, which had been believed to reduce the adverse effects on kidney function of contrast agents used in angiography, was found to be any more beneficial than using saline alone.
The results were published recently in the New England Journal of Medicine.1
“Both of these treatments are used in hospitals all over the world with the belief that they are helping patients,” explained lead author Steven Weisbord, MD, a nephrologist with the VA Pittsburgh Healthcare System and University of Pittsburgh School of Medicine, both in Pittsburgh.
He added that the treatments don’t appear to be harmful but, “our results suggest that patients should instead just be treated with saline which is both cheaper and more readily available.”
Intravenous sodium bicarbonate and oral acetylcysteine have been used for 15 years to prevent acute kidney injury and associated adverse outcomes after angiography without definitive evidence of their efficacy, according to the article.
To remedy that, Weisbord and his colleagues randomly assigned about 5,000 patients at high risk for renal complications and who were scheduled for angiography to receive intravenous 1.26% sodium bicarbonate or intravenous 0.9% sodium chloride, as well as five days of oral acetylcysteine or oral placebo. Patients in the study, which was an international collaboration involving the VA, were from the United States, Australia, New Zealand and Malaysia.
A composite of death, the need for dialysis or a persistent increase of at least 50% from baseline in the serum creatinine level at 90 days was defined as the primary outcome with contrast-associated acute kidney injury a secondary end point.
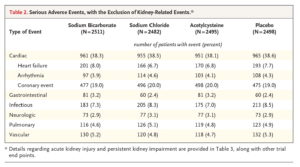
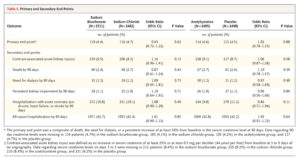
With the trial ended after a prespecified interim analysis, researchers detected no interaction between sodium bicarbonate and acetylcysteine as to the primary end point. The primary end point occurred in 110 of 2511 patients (4.4%) in the sodium bicarbonate group vs. 116 of 2482 (4.7%) in the sodium chloride group for an odds ratio of 0.93.
At the same time, the primary end point occurred in 114 of 2495 patients (4.6%) in the acetylcysteine group, compared with 112 of 2498 (4.5%) in the placebo group, for an odds ratio of 1.02. Study authors said that mean “no significant between-group differences in the rates of contrast-associated acute kidney injury.”
“Among patients at high risk for renal complications who were undergoing angiography, there was no benefit of intravenous sodium bicarbonate over intravenous sodium chloride or of oral acetylcysteine over placebo for the prevention of death, need for dialysis, or persistent decline in kidney function at 90 days or for the prevention of contrast-associated acute kidney injury,” the researchers concluded.
“This definitive study has shown that these treatments are not helping people avoid acute kidney failure nor the other poor outcomes that result from this complication. In addition, they are adding unnecessary complexity and cost,” pointed out co-author Martin Gallagher, MBBS, PhD, of The George Institute for Global Health in Australia.
Patients with history of kidney disease, heart failure or diabetes are considered to have a higher risk of renal complications from angiography, which are associated with longer hospital stay, higher mortality and worsening of kidney function.
- Weisbord SD, Gallagher M, Jneid H, Garcia S, Cass A, Thwin SS, Conner TA, Chertow GM, Bhatt DL, Shunk K, Parikh CR, McFalls EO, Brophy M, Ferguson R, Wu H, Androsenko M, Myles J, Kaufman J, Palevsky PM; PRESERVE Trial Group. Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine. N Engl J Med. 2017 Nov 12. doi: 10.1056/NEJMoa1710933. [Epub ahead of print] PubMed PMID: 29130810.