BALTIMORE, MD—A post-hoc analysis of the Veterans Affairs Diabetes Trial (VADT) once again shines a spotlight on the dangers of hypoglycemia in veterans treated for Type 2 diabetes.
The study published in Diabetes Care found that severe hypoglycemic episodes within the previous three months were associated with increased risk for major cardiovascular events and cardiovascular and all-cause mortality, and that was the case whether patients were treated with intensive or standard glycemic therapy.1
The authors also reported that even standard therapy further increased the risk for all-cause mortality after severe hypoglycemia.
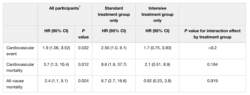
Table 3
Increased risk of cardiovascular events and mortality associated with severe hypoglycemia within the prior 3 months
*Adjusted for treatment group, cardiovascular risk (as estimated by UKPDS score), history of cardiovascular event, insulin at baseline, and eGFR.
“In this study, we report that the association of severe hypoglycemia with the risk of all-cause mortality was significantly increased in the standard glycemic treatment group compared with the intensive treatment group,” the authors wrote, noting that the finding is in line with earlier studies, which found that participants in the standard arm who had experienced severe hypoglycemia had a significantly higher relative risk of death. “Thus, severe hypoglycemia appears to carry an additional risk in individuals with higher HbA1c values and who may be attempting intensification of glucose-lowering therapy, at least in older participants with more advanced diabetes.”
VADT was a randomized controlled multicenter study that investigated the effects of intensive glycemic control on macrovascular and microvascular complications in veterans with T2DM.2 This post-hoc analysis specifically looked at the association between severe hypoglycemia and a major cardiovascular event—a composite of myocardial infarction, stroke, death as a result of cardiovascular causes, congestive heart failure, surgery for vascular disease, inoperable coronary artery disease and amputation for ischemic gangrene—and whether that association varied with intensive vs. standard treatment assignment and the extent of initial cardiovascular disease risk.
The follow-up included 1,791 military veterans, median age 60.5, with sub-optimally controlled Type 2 diabetes, a median hemoglobin A1c of 9.4%, and a mean of 11.5 years of disease duration from 20 VAMCs across the country. The participants, who were with and without known cardiovascular disease and additional cardiovascular risk factors, were randomized to either intensive glucose control, with an HbA1c goal of lower than 7% or standard treatment seeking to lower HbA1c to less than 8.5%.
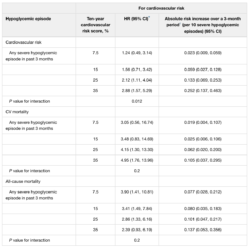
Table 4
Association of severe hypoglycemia with cardiovascular events and cardiovascular mortality by baseline cardiovascular risk
*A statistically significant increase in the relative association (HR) of severe hypoglycemia with CVD risk (as measured by the UKPDS risk engine) was found for major CVD events.
†The absolute risk of adverse events increased greatly with higher CVD risk for all three outcomes. Models include treatment group, severe hypoglycemia in prior 3 months, UKPDS risk, and the UKPDS × severe hypoglycemia interaction. Estimated using UKPDS risk engine.
Results indicated that the rate of severe hypoglycemia in the intensive treatment group was 10.3 per 100 patient-years compared with 3.7 per 100 patient-years in the standard treatment group. After analysis, researchers found that insulin use at baseline (P= 0.02), proteinuria (P= 0.009) and autonomic neuropathy (P= 0.01) were independent risk factors for severe hypoglycemia, although higher body mass index was protective (P= 0.017).
Serious Cardiovascular Events
In addition, the study team reported that severe hypoglycemia within the past three months was associated with an increased risk of serious cardiovascular events (P = 0.032), cardiovascular mortality (P= 0.012) and total mortality (P= 0.024).
Of note, the study emphasized that a relatively greater increased risk for total mortality was documented in the standard group vs. the intensive group (P= 0.019). Researchers added that the association between severe hypoglycemia and cardiovascular events increased significantly as overall cardiovascular risk increased (P= 0.012).
In both study groups, patients with a BMI of 27 kg/m2 or greater were started on two oral agents, metformin plus rosiglitazone, while those with a lower BMI were initiated with glimepiride plus rosiglitazone. A key difference in the groups was that patients undergoing intensive therapy group were started on maximal doses, and those on standard therapy were started on one-half the maximal doses.
Before any change in oral medications, insulin was added for patients in the intensive therapy group who did not achieve HbA1c of less than 6% and for those in the standard therapy group with a level greater than 9%. Study authors pointed out that an absolute HbA1c separation of 1.5% or greater was to be maintained between the therapy groups.
At each three-month study visit, researchers recorded the number of severe hypoglycemic episodes—defined as a self-reported episode of a low blood glucose value accompanied by confusion requiring assistance from another person or loss of consciousness—since the last visit.
The study noted that hypoglycemia is associated with several electrocardiogram changes, including ST-segment depression consistent with ischemia, heart rate variability and QT prolongation that can be associated with arrhythmias and increased mortality. Other effects of hypoglycemia include increased blood viscosity, enhanced platelet aggregation, increased plasminogen activator inhibitor-1, thromboglobulin, coagulation factor VIII, Von Willebrand factor, and thrombin generation. “All these create a hypercoagulable and atherothrombotic state that increases cardiovascular risk,” the researchers wrote.
“Although the explanation for the relatively greater risk of serious adverse events after severe hypoglycemia in the standard treatment group is unknown, we agree with previous reports that milder episodes of hypoglycemia, which are more frequent in the intensive treatment group, may quantitatively blunt the release of neuroendocrine and autonomic nervous system responses and their resultant metabolic and cardiovascular responses to hypoglycemia, thereby lessening the impact of subsequent severe hypoglycemic episodes,” the authors explained.
“On the other hand, an isolated severe hypoglycemic event in a less well-controlled individual could provoke a relatively greater counterregulatory response with a proportionally attendant elevated risk for adverse vascular effects,” they added.
What does this mean for T2D treatment at the VA?
“The serious consequences of these hypoglycemia-associated outcomes (cardiovascular events and mortality) emphasize the importance of careful selection of patients and medications when initiating intensification of therapy and close monitoring of patients for evidence of these events,” wrote the authors. “We have identified several clinical characteristics that increased the risk of severe hypoglycemia in the VADT. These included insulin use, proteinuria (a marker of reduced renal function and, therefore, reduced insulin clearance) and autonomic neuropathy. Several of these have been identified before and confirm the importance of factoring in these clinical characteristics when selecting glucose targets and therapy approaches.”
The researchers also underscored that greater BMI provided a protective effect against severe hypoglycemia “perhaps because of the associated insulin resistance providing some protection against the glucose-lowering effects of insulin or insulin secretagogues.”
The study pointed out that, while baseline HbA1c levels were not a significant multivariable predictor of severe hypoglycemia in the whole group, “there was a significant association in the standard group and a strong trend in the intensive group for greater frequency of episodes in participants with higher initial values. This seems paradoxical, but it may be that higher HbA1cc levels also identify patients with more variation in glucose levels who are, therefore, more likely to become hypoglycemic with any attempt at intensification of glycemic control.”
A specific alert applied to a group of patients routinely treated by VA primary care physicians and endocrinologists. The study team cautioned about patients who are working to improve glycemic control but have HbA1c values of 9% to 10% and are having trouble lowering their levels. “These individuals, whether in intensive or standard treatment groups, have an increased risk of serious adverse events after severe hypoglycemia and were the group most at risk for mortality after severe hypoglycemia” in previous studies, the researchers warned.
The report also described how recent hypoglycemia “may provide an acute stress event that is most harmful to those already predisposed to a cardiovascular event.”
1. Davis SN, Duckworth W, Emanuele N, et al., for the VADT investigators. Effects of severe hypoglycemia on cardiovascular outcomes and death in the Veterans Affairs Diabetes Trial. Diabetes Care. 2019;42(1):157-163. doi.org/10.2337/dc18-1144
2. Duckworth W, Abraira C, Moritz T, et al., for the VADT investigators. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009; 360(2):129-139. doi: 10.1056/NEJMoa0808431.