ANN ARBOR, MI—New prognostic models developed by VA researchers can help clinicians identify which patients who have or have had chronic hepatitis C virus infection will develop cirrhosis or hepatocellular carcinoma.
While the VA has nearly eliminated HCV among veterans, the predictive models come at a critical juncture for public health as the number of new HCV infections has risen sharply in recent years as a result of the opioid abuse epidemic. After dropping from a peak of 291,000 in 1989 to 16,000 in 2010, new infections rebounded to 41,200 in 2016 and continue to climb, the Centers for Disease Control and Prevention recently reported. An estimated 2.4 million Americans currently live with chronic HCV.
About 20% of individuals who contract hepatitis C spontaneously clear the infection. Of those with chronic infection, 10% to 15% eventually develop cirrhosis. Patients with cirrhosis have a 1% to 5% annual risk of developing hepatocellular carcinoma and a 3% to 6% annual risk of hepatic decompensation, according to the CDC.
“Right now, we can only identify patients at risk once they have already developed advanced fibrosis, but using our methodology, we are seeking to prognosticate and identify those at risk prior to them developing advanced fibrosis,” said Akbar K. Waljee, MD, director of the Inflammatory Bowel Disease Program at the VA Ann Arbor Healthcare System, associate director of the Michigan Integrated Center for Health Analytics and Medical Prediction and associate professor in internal medicine at the University of Michigan.
Waljee is a co-author of the study that evaluated the predictive ability of longitudinal and cross-sectional models of HCV progression using machine learning. The study appeared in PLOS ONE earlier this year.1
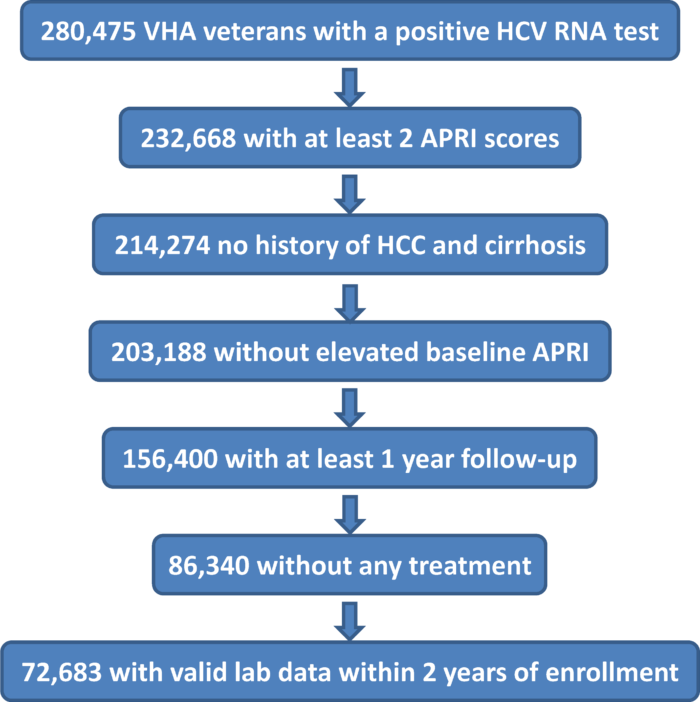
The study included 72,683 veterans with chronic HCV who received care through the VA between 2000 and 2016 but had not received antiviral therapy. Of those, 11,616 developed cirrhosis over a mean follow-up period of seven years.
While the longitudinal boosted-survival-tree model had the best predictive performance, all four models evaluated represented a substantial improvement compared to current prognostic methods. Concordance ranged from 0.746 to 0.774.
Some of the models could be implemented fairly easily, Waljee told U.S. Medicine, particularly at the VA, which has a robust electronic health record system that can be leveraged to make better predictions. Other systems may have difficulty operationalizing a model that requires input of longitudinal data, so for them, the cross-sectional models might be simpler to implement.
“The difference in predictive ability between longitudinal and cross sectional models depends on cohort evaluated and disease. In this case, all were all better than the usual methods, which predict outcomes at the very end of liver disease,” said co-author Grace Su, MD, associate chief of Medicine for Subspecialty Care and Access and chief of the Gastroenterology Section of the VA Ann Arbor, MI, Healthcare System and professor of internal medicine and surgery at the University of Michigan.
In addition to demonstrating the feasibility of creating “highly accurate models for risk of progression to cirrhosis at varying time intervals of interest” for patients with untreated HCV, the study also illustrated the advantages of using machine learning algorithms to better understand other non-linear, dynamic disease states, the authors noted.
Modeling HCC Risk
The team acknowledged the need for another model that addressed the risks facing previously treated patients, as well.
“Assessing the risk of liver disease progression among patients who had successfully treated chronic hepatitis C would be of particular relevance to current clinical practice to help guide the level of monitoring for liver disease progression of patients thereafter,” Waljee said.
Achieving sustained virologic response reduces the risk of hepatocellular carcinoma, ascites, encephalopathy and variceal bleeding, but “in patients who had already developed advanced fibrosis or cirrhosis before eradicating chronic hepatitis C, a residual risk of these complications unfortunately persists,” Waljee explained. For those patients, current guidelines recommend continued screening for HCC indefinitely, he added, creating “an incredible strain on resources, physicians and patients.”
The research team said it hopes to develop models to identify which patients remain at risk of developing HCC after SVR, whether the risk declines over time and at what point, if any, screening could safely be discontinued.
While the rate of HCC is lower in patients who achieved SVR and did not have cirrhosis, it is not insignificant, but guidelines do not recommend screening these patients at all. And how should physicians proceed with patients who received treatment for HCV and did not achieve SVR?
Some members of the machine-learning model research team and other VA colleagues have tackled part of this challenge. They developed an online tool (www.hccrisk.com) that can help clinicians better tailor surveillance strategies to patients who have received HCV treatment.2
Led by George Ioannou, MD, MS, of the VA Puget Sound Healthcare System and professor of gastroenterology at the University of Washington in Seattle, this second VA group studied 45,810 veterans who received treatment for HCV through the VA between 2009 and 2015. Patients could have received direct acting antivirals (64%) or interferon with or without direct acting antivirals (36%). Almost one-quarter of patients had cirrhosis at the time of treatment and 74% achieved SVR.
The researchers followed patients until June 15, 2017, for a mean follow-up period of 2.5 years, and identified 1,412 incident cases of HCC diagnosed at least 180 days after beginning antiviral treatment.
The team developed predictive models tailored to patients in four groups, those who achieved SVR and had cirrhosis, those who attained SVR and did not have cirrhosis, patients who did not achieved SVR and had cirrhosis and patients who did not achieve SVR and did not have cirrhosis.
They determined that four easily obtained factors accounted for most of the variation in risk within the subgroups: age, platelet count, serum aspartate aminotransferase/alanine aminotransferase ratio and albumin levels. The models also included six other predictors that had less impact on outcomes.
Future Approaches
While the prognostic models developed at the VA have immediate use in public health and veteran care, the researchers suggested that the overall approach to HCV treatment in the U.S. might take a very different direction in the coming years that could make them less important. That approach could look a lot like what the VA has done already.
“The VA has done a phenomenal job trying to treat all veterans with hepatitis C, and it is on its way to treating all those who are candidates for treatment. The VA should be a model for how to treat all patients with hepatitis C,” Waljee said.
“We have a very effective drug, nearly a miracle, and we are able to treat patients with very few side effects. We should be preemptively treating patients,” Su noted. “Our paper doesn’t address this at all, but infectious disease physicians have presented the idea of preventive treatment, where patients take medication right after exposure, similar to the HIV model.”
Treating recently infected patients across the board has a major downside—the high cost of treatment. It also has a real upside, Su said, in terms of significantly reducing the spread of the virus.
Ioannou agreed. “We could ignore [recently infected patients] for the time being, but who is spreading those infections? Probably not the person who has had it for 30 or 40 years, they are much less likely to have high risk behaviors.”
The benefit of predictive models that help identify the sickest patients or those most likely to become sick in the future is clear.
“This is a more controversial approach,” said Ioannou, “but five years ago, there were contraindications to treating patients likely to be reinfected. Now the VA is looking to treat those with substance use disorders and the homeless. Perhaps we should be thinking of both at the same time—treating those at highest risk those most likely to spread the virus. Who knows where we’ll be in another five years.”
Konerman MA, Beste LA, Van T, Liu B, Zhang X, Zhu J, Saini SD, Su GL, Nallamothu BK, Ioannou GN, Waljee AK. Machine learning models to predict disease progression among veterans with hepatitis C virus. PLoS One. 2019 Jan 4;14(1):e0208141.
Ioannou GN, Green PK, Beste LA, Mun EJ, Kerr KF, Berry K. Development of models estimating the risk of hepatocellular carcinoma after antiviral treatment for hepatitis C. J Hepatol. 2018 Nov;69(5):1088-1098.

