CINCINNATI — The VA is leveraging its position as the country’s largest integrated healthcare system to slow the development and spread of multidrug-resistant organisms (MDRO).
The need for leadership is critical; in April, the national Centers for Disease Control and Prevention announced the identification within the U.S. last year of 221 instances of unusual resistance genes in ”nightmare bacteria.”
”CDC’s study found several dangerous pathogens, hiding in plain sight, that can cause infections that are difficult or impossible to treat,” said CDC Principal Deputy Director Anne Schuchat, MD. A quarter of the pathogens tested by the CDC’s antibiotic resistance lab network in 2017 had features that enabled them to easily spread resistance mechanisms to unrelated bacteria. Screening tests discovered highly resistant germs in 11% of asymptomatic patients.
”Multidrug-resistant organisms cause infections that are very difficult to treat. This threat goes beyond the medical community. It is a public health crisis waiting to happen,” explained Eli Perencevich, MD, MS, director of the Center for Comprehensive Access & Delivery Research and Evaluation (CADRE) at the Iowa City Veterans Affairs Health Care System. ”The Veterans Health Administration is uniquely positioned to be a leader in this area and has the ability to make a real impact.”
In 2016, the VA assembled experts in antimicrobial stewardship, medical anthropology, clinical medicine, epidemiology, infection prevention, pharmacy and sociology to identify the most important areas for future research in MDROs. This spring the group released four papers, each of which tackled a different, critical topic—transmission dynamics, antimicrobial stewardship, microbiome and special populations. The papers were published in Infection Control & Hospital Epidemiology.
The papers and collaborative approach to identifying the most urgent research needs continues a long-standing focus at the VA. ”We were taking steps to control the spread of resistant organisms before most people were even thinking about it,” said Gary Roselle, national director of the VA’s Infectious Diseases Service and professor of medicine at the University of Cincinnati College of Medicine.
The VA implemented a bundle of activities to control transmission of methicillin-resistant Staphylococcus aureus (MRSA) in acute care settings in 2007. Control steps included nasal surveillance, contact precautions, hand hygiene and significant changes in institutional culture that included hiring a MRSA coordinator at each facility and encouraging innovation from staff on the floors and at bedside. In 2012, a Clostridium difficile initiative built on the success of the MRSA program, according to the transmission dynamics paper. A directive outlining steps to control carbapenem-resistant Enterobacteriaceae (CRE) followed in 2014, with an update in 2017.1
The VA’s programs have been effectively implemented and maintained for years. ”I can do almost anything for six months. Sustainability is the key to success,” Roselle told U.S. Medicine. A number of papers published over the past decade in leading medical journals have documented the program’s continued success.
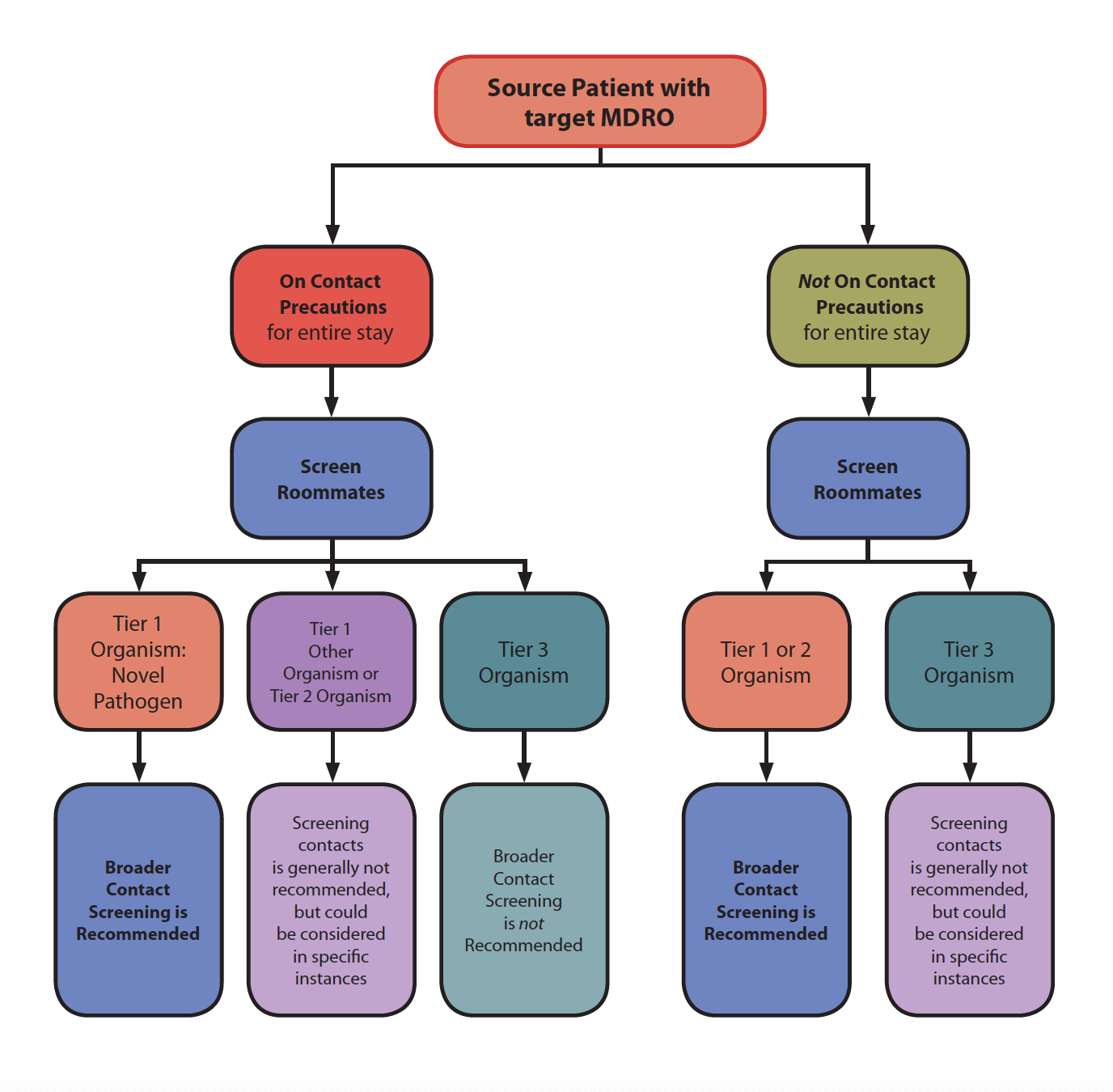
The article on transmission dynamics drew on the existing VA programs and evaluated various pathogen-targeted initiatives to determine what aspects work well and where improvement may be appropriate, such as how to more accurately measure and improve hand hygiene and whether active or targeted surveillance should be added to the CDI and CRE directives, and the efficacy of environmental cleaning technologies.
In terms of antimicrobial stewardship, Roselle said that he and other leaders at the VA ”try to think about what’s going to be the next big thing two years from now so we can get ahead of it.” As part of that effort, the VA required every hospital to have an antimicrobial stewardship program (ASP) jointly led by a pharmacist and a medical officer beginning in 2014, making it one of the first organizations to do so.
”Often the pharmacist is the linchpin in the local organization. For a pharmacist, leading an ASP can be very rewarding and effective,” Roselle said. ”There’s not an abundance of infectious disease [specialists] or pharmacists who are specifically excited about stewardship,” he added. ”The VA’s working on training more pharmacists” to fill the gap.
While programs led by physicians or pharmacists who specialize in infectious disease have proved successful at optimizing appropriate use of antimicrobials, those specialists are in short supply and high demand, making it unfeasible to have one head each hospital’s ASP. The research agenda for ASPs calls for an evaluation of how best to provide infectious disease resources to a wider group and how else to effectively staff ASPs, along with an examination of the core components of an ASP and best metrics for determining success.2
Education has continued to be a critical component of the antimicrobial stewardship program, according to Roselle. ”We have a number of webinars, and their popularity has not decayed in terms of the number of people watching over the years.” Resources included information on how to avoid double coverage of anaerobics, extensive guidance of antimicrobial selection and materials to support local implementation.
”Stewardship a lot more individualized than other things we do. You can say, ‘Don’t use this antibiotic,’ but we want to make sure we don’t have unexpected harm from doing that,” Roselle said.
The challenge can be even greater in a nonacute setting, where physicians have less information on the patient. ”Someone comes in; you think it’s sinusitis. If you read recommendations, they say most people do not get antibiotics and it goes away, but there are caveats. For a patients with chronic lung disease, it’s not so clear. A patient population like ours has to be carefully done,” he explained.
Overall, Roselle expects sustaining efforts to control MDROs to be more difficult than getting programs up and running, whether in hospitals or in ambulatory or long-term facilities. ”We need to ensure sustainability locally and an overall commitment across the country in all healthcare systems as well as implement international control. Combating resistance and spread of MDROs works best as a massive, ongoing program that’s done across the board.”
