WASHINGTON—Zika virus infection had affected more than a half-million people in the Western Hemisphere by the end of 2016. Among those were more than 700 VA patients with confirmed or presumed possible infection.
Much of the concern was about the effects on unborn fetuses or young women seeking to become pregnant, with the assumption that ZIKV infection’s effects were generally mild in everyone else. The new article, published in PLOS Neglected Tropical Diseases, raised questions, however, about the danger of Zika in an older population with significant co-morbidities.1
To help add to the understanding of which patients are most at risk of severe disease from ZIKV infection, researchers from Public Health Surveillance & Research at the VA described risk factors for hospitalizations and neurologic complications among veterans.
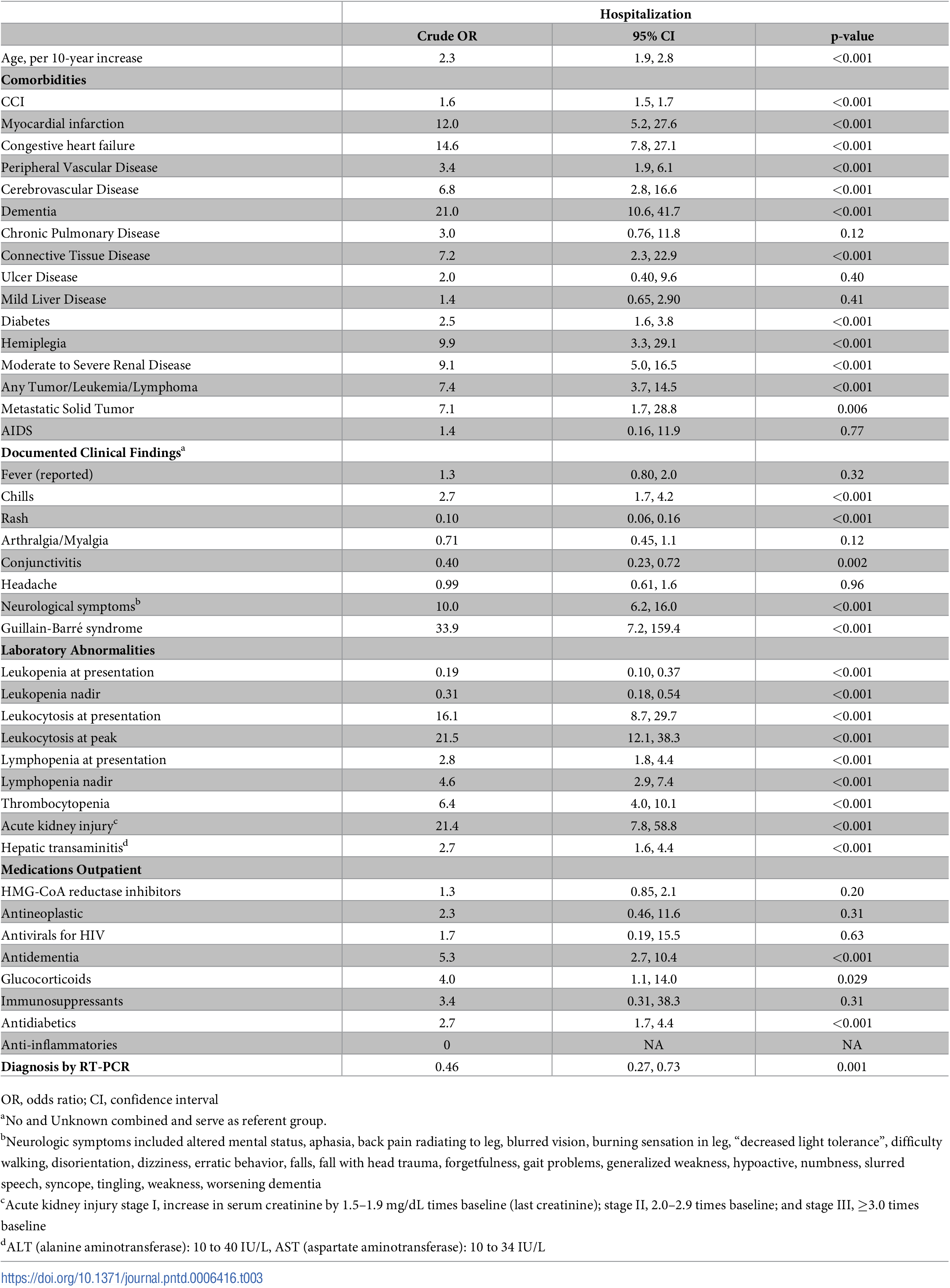
The study found that older veterans with multiple comorbidities, as well as those presenting with neurologic symptoms, were more likely to be hospitalized. Interestingly, patients presenting with rashes were less likely to be hospitalized, according to the report.
In addition, researchers report that patients who were hospitalized or had a prior history of cerebrovascular disease or dementia were more likely to develop neurologic complications.
“Better understanding of those patients most at risk for severe disease can help providers when evaluating and treating patients with ZIKV infection,” study authors wrote.
“Hospitalization and deaths are reported to be uncommon in ZIKV infection,” researchers added. “During the 2007 ZIKV outbreak in Micronesia, among 49 confirmed and 59 probable cases, patients presented with typical symptoms described here, but none were hospitalized, and none died. Although patients in that study were on average >10 years younger, fewer had comorbidities than U.S. veterans. In Brazil, among 119 ZIKV confirmed patients, only one hospitalization and no deaths were reported]. Hospitalizations and death (<1%) were noted in Puerto Rico from November 2015-July 2016. In our veteran population, 3% died after a ZIKV diagnosis, and 13% were hospitalized, which is higher than other ZIKV studies and may be related to veterans increased comorbidities.
An outbreak of ZIKV, a flavivirus transmitted primarily by Aedes mosquitos, occurred in 2015 and 2016, affecting hundreds of thousands of people, including more than 5,000 cases in the continental United States and more than 36,000 in Puerto Rico and the Virgin Islands. Because VHA has healthcare facilities throughout the United States and its territories, it was an ideal location to perform ongoing surveillance for emerging pathogens, the study suggested.
For the recent study, researchers conducted a case series study of all ZIKV cases in VHA hospitals in 2015 and 2016, analyzing patient characteristics and clinical outcomes of 736 ZIKV positive patients out of the 1,538 patients who were tested for ZIKV during that time.
Over, 736 (48%) of the patients tested positive for ZIKV. Most, 89%, were male, and the great majority, 93%, were treated by the VA Caribbean Healthcare System. The remaining 7% of patients were diagnosed at 24 other VHA medical centers.
Documented Travel
Documented travel for those diagnosed in the continental United States included non-Puerto Rico Caribbean (18), Puerto Rico (16), Central America (9), South America (2), Indonesia (1) and Senegal (1), while six patients had exposure only in Florida.
Mean age of all patients was 58.8 years (range 20-99), although patients from the VA Caribbean Healthcare System compared to returning travelers with ZIKV infection were older (mean age 60 vs. 47).
Hospitalization was necessary for 13% of the patients, and 3% died after their ZIKV infection.
Results indicated that hospitalization was associated with:
- Increased Charlson co-morbidity index (adjusted odds ratio [OR] 1.2; 95% confidence interval [CI], 1.1-1.3);
- Underlying connective tissue disease (OR, 29.5; CI, 3.6-244.7);
- Congestive heart failure (OR, 6; CI, 2-18.5);
- Dementia (OR, 3.6; CI, 1.1-11.2);
- Neurologic symptom presentation (OR, 3.9; CI, 1.7-9.2);
- Leukocytosis (OR, 11.8; CI, 4.5-31);
- Thrombocytopenia (OR, 7.8; CI, 3.3-18.6);and
- Acute kidney injury (OR, 28.9; CI, 5.8-145.1), or using glucocorticoids within 30 days of testing (OR, 13.3; CI 1.3–133).
Patients presenting with rash were less likely to be hospitalized (OR, 0.29; CI, 0.13–0.66), however.
Researchers also reported that risk for neurologic complications increased with hospitalization (OR, 5.9; CI 2.9-12.2), cerebrovascular disease (OR 4.9; CI 1.7-14.4), and dementia (OR 2.8; CI 1.2-6.6).
“ZIKV has been documented to have congenital as well as neurologic complications,” the study authors wrote. “Forty-six patients in our cohort were also noted to have neurologic complications after ZIKV infection. While these neurologic complications are quite broad, they identify potential complications post-ZIKV infection. Prior history of CVD and dementia as well as being hospitalized with ZIKV increased risk of neurologic complication. It was difficult to confirm whether these other neurologic complications were the result of ZIKV infection. Since neonatal and pediatric care was not provided by VA, the status of the infants exposed to ZIKV is unknown.”
1. Schirmer PL, Wendelboe A, Lucero-Obusan CA, Ryono RA, et. Al. Zika virus infection in the Veterans Health Administration (VHA), 2015-2016. PLOS Neglected Tropical Diseases, 2018; 12 (5): e0006416 DOI: 10.1371/journal.pntd.0006416

