WASHINGTON–A survey of veterans receiving mental healthcare through VA found that the vast majority would favor at least one option to restrict firearm access with the goal of reducing dangers of self-harm.
Cleveland EC, Azrael D, Simonetti JA, Miller M. Firearm ownership among American veterans: findings from the 2015 National Firearm Survey. Inj Epidemiol. 2017;4(1):33. Published 2017 Dec 19. doi:10.1186/s40621-017-0130-y
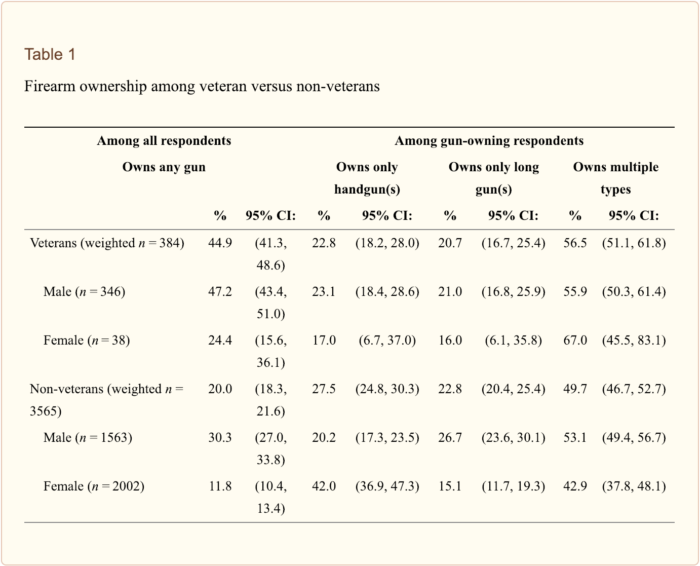
Research shows that veterans are approximately 50% more likely than civilians to commit suicide, with the majority of them (70%) using a gun to do so. However, with recent statistics showing an increase in suicides among younger veterans, VA officials caution against focusing solely on mental health issues as the sole cause of suicide.
The survey, funded by the VA Health Services Research and Development Service and the VA Center for Excellence for Suicide Prevention, asked detailed questions of 660 veterans currently receiving mental health treatment at five VA facilities. They were given gun safety options, ranging from low-intensity interventions like having clinicians ask about access to firearms and distribution of gunlocks to higher-intensity interventions, such as assisting veterans with storing or disposing of their guns and helping families secure veterans’ guns.1
More than 93% of respondents supported one or more interventions, with 75% endorsing limitations substantially reducing access. Veterans with household firearms were less likely to endorse interventions, but, still, more than 50% said they would personally participate in an intervention that substantially limited gun access.
“Veterans in mental healthcare are in favor of voluntary programs to reduce firearm access during high-risk periods. This suggests the VA and other health systems should consider working with veterans to develop and implement these programs,” explained study author Marcia Valenstein, MD, MS, a member of the University of Michigan Institute for Healthcare Policy and Innovation and the VA Center for Clinical Management Research. “Half of veterans in mental healthcare indicated that, if they were suicidal, they would participate in interventions that would substantially limit their own access to their firearms.”
According to the study, the higher rate of gun ownership among veterans can be linked to the higher rate of suicide, with the presence of firearms in the house making it easier to turn ideation into reality. Two-thirds of veterans surveyed said that they might or definitely would be open to VA offering storage or disposal options during times when they might be at a higher risk of suicide.
The survey comes on the heels of newly-released statistics showing an increase in suicide among veterans aged 18-34. A report released by VA in October shows that, while overall the number of veteran suicides decreased slightly between 2015 and 2016—the latest year data is available—suicides among the youngest cohort of veterans rose 10%.
Speaking at a panel organized by the Wounded Warrior Project, Keita Franklin, director of VHA’s Office of Mental Health and Suicide Prevention, cautioned against developing tunnel vision when it comes to suicide prevention.
“Healthcare is critically important to get people in the door at the right time and the right place when they need it most, but it’s bigger than that,” Franklin said. “We’re looking at all social aspects—VA performing as a vehicle to connect veterans with veterans service organizations and peer support.”
Having access to a social network and to meaningful employment or volunteer work can be just as important as mental healthcare, she noted.
“We’re seeing in the suicide data the importance of social media for support. Veterans in particular will, even when they’re at risk and struggling, post on a public platform,” she noted. “Having good internet access improves lives.”
Meaningful employment can also be a protective factor against suicide, Franklin said. “Financial risk factors are important. We see it playing out more and more in our data. That wasn’t how it was when I first entered the field. We thought of it as a mental health problem, with divorce sometimes coming into play. But now we see that falling from glory and having trouble with your finances can be an important risk factor. If we can’t get you meaningful and purposeful employment, can we get you involved in volunteer-based activities?”
That the increase is being seen among the youngest veterans suggests to Franklin that there’s more than VA and DoD can do during the transition process to keep tabs on a veteran’s well-being. Asked about the viability of VA conducting periodic health assessments for veterans in the same way that DoD does for active duty servicemembers. “The work of transitioning between VA and DoD is so important. That the rate has increased 10% for 18-34 year olds, we think it might have something to do with making sure we’re transitioning them well. There might be something more we can do.”
1. Valenstein M, Walters H, Pfeiffer PN, Ganoczy D, Miller M, Fiorillo M, Bossarte RM. Acceptability of potential interventions to increase firearm safety among patients in VA mental health treatment. Gen Hosp Psychiatry. 2018 Nov -Dec;55:77-83. doi: 10.1016/j.genhosppsych.2018.10.010. Epub 2018 Nov 3. PubMed PMID: 30447477.

I have this conversation with all my vets and it usually goes over like a lead balloon.
I begin by stating I support 2A, have weapons myself, BUT that it is also a great responsibility.
Please consider WHY you need guns. If you only hunt or target shoot, then let a friend or family member keep them under lock and key. Use them when feeling ok, clean them and put them away.
For those who claim to be Libertarians, I ask them how it is philosophically consistent to reject Gov’t rules and regs, own a firearm, yet depend on Big Gov’t for a check from the taxpayers (who might question why someone ‘disabled’ for mental health purposes can still own a weapon)
Somehow they never seem to see that contradiction.
So, we’ll just end up with more preventable gun deaths. Great.