NEW YORK—The VA is taking a leading role in use of conservative treatment for veterans diagnosed with non-aggressive prostate cancer.
Noting that low-risk prostate cancer generally has a favorable prognosis without treatment, current clinical guidelines often recommend conservative management or deferring upfront treatment as the preferred approach.
That advice is often not followed in the United States, according to a research letter published recently in JAMA, at least partly because financial incentives and legal concerns work against it.1
Those aren’t as much of an issue at the VA, however, because the integrated healthcare system—the nation’s largest—provides equal access for patients without financial incentives for physicians to provide high-volume care, the study pointed out.
A study team led by researchers from the Manhattan campus of the VA New York Harbor Healthcare System and NYU School of Medicine found that, instead, increasing numbers of veteran patients are opting to postpone additional therapy unless their symptoms worsen—a watchful waiting. Others are electing active surveillance in which regular check-ups, including blood tests, physical exams and the occasional needle sampling of prostate tissue, monitor to determine if and when aggressive treatment might be considered.
Investigators used VA’s Central Data Warehouse to analyze treatment patterns for veterans diagnosed with low-risk prostate cancer—prostate-specific antigen (PSA) less than 10 ng/mL, Gleason score six or under and staged at cT1/T2a—from January 2005 through November 2015.
The goal was to determine whether curative therapy, including androgen deprivation monotherapy, was received within one year of diagnosis. The team not only looked at VA administrative codes but also examined Medicare records in case tests or treatment performed outside the VA for men 65 years or older; the JAMA article noted that men with PSA less than 1 ng/mL during follow-up were also considered as likely having received curative treatment outside the VA.
Untreated veterans were classified as receiving conservative management, divided into two groups: active surveillance, involving two or more PSA tests and one biopsy within two years after diagnosis, or watchful waiting, with Nov. 16, 2017, being the final date of follow-up.
Low-risk prostate cancer was determined in 125, 083 veterans, who had a mean age of 6 and mean PSA of 5.4 ng/mL (SD, 2.1). Slightly more than half, 52%, had been treated—65% identified through VA claims, 25% by PSA less than 1 ng/mL and 10% through Medicare claims.
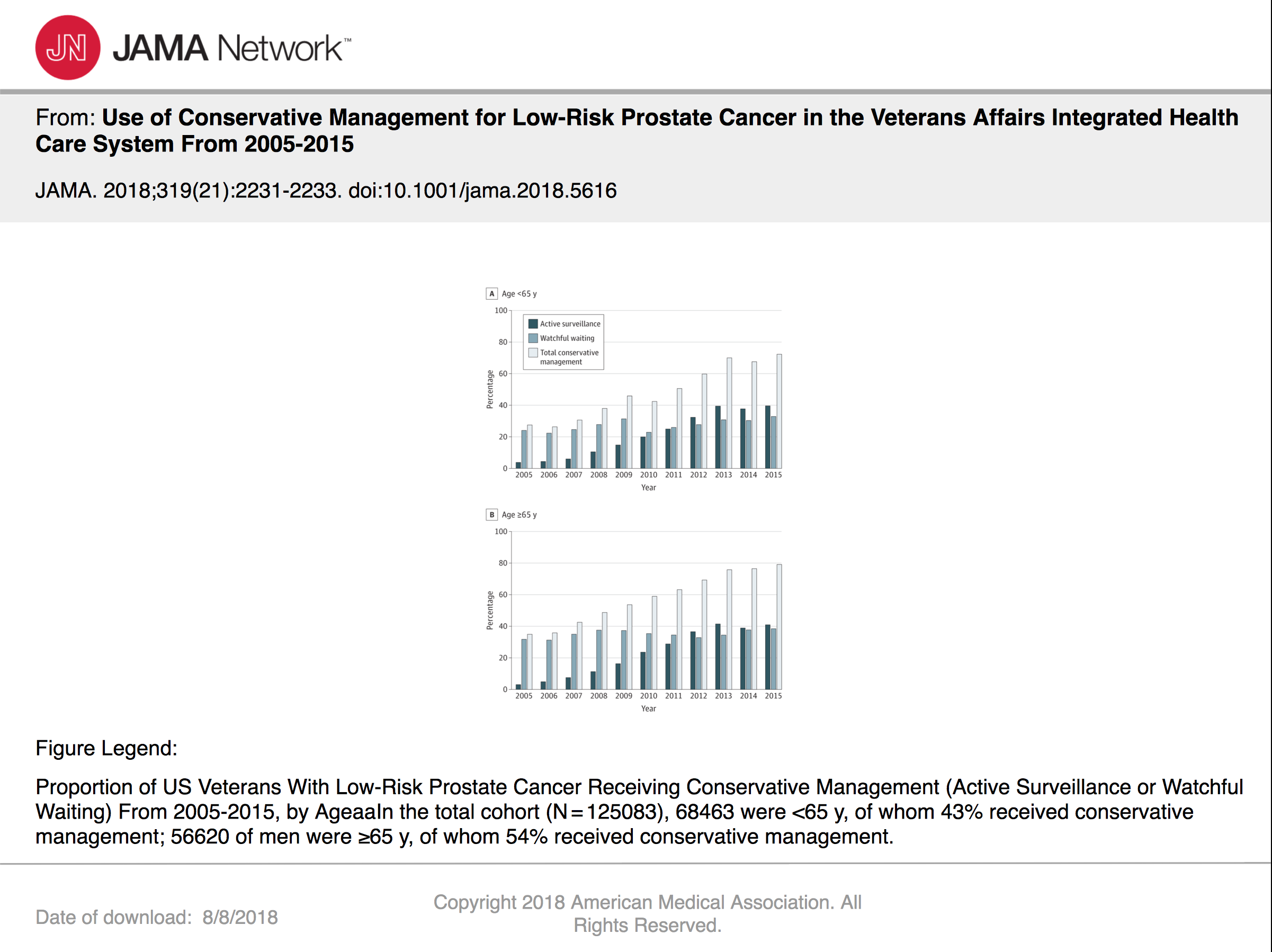
Results indicated that use of conservative management increased among men younger than 65 years (27% in 2005 to 72% in 2015) and 65 years or older (35% in 2005 to 79% in 2015. Researchers suggested the increase was primarily due to greater use of active surveillance—4% in 2005 to 39% in 2015 in men younger than 65 and 3% in 2005 to 41% in 2015 in men 65 or older.
After analysis, the study team determined that more recent years were associated with greater odds of conservative management, as were increasing age, black race, unmarried status, higher PSA, increasing comorbidity and geographic region. Watchful waiting was more likely in men older than 75 years, as well as those with higher PSA and greater comorbidity, compared to active surveillance, the study found.

“Our study shows that the Veterans Affairs healthcare system has done a good job over the last decade in adopting ‘conservative management’ of men diagnosed with early-stage disease, with many men choosing active surveillance as an alternative to immediate therapy,” explained the study’s senior investigator Stacy Loeb, MD, MSc, an attending urologist at VA New York Harbor Healthcare System and an assistant professor in the urology and population health departments at NYU School of Medicine.
“This marks a historic reversal, at least at the VA, in the decadeslong overtreatment of men with prostate cancers least likely to cause harm and brings their care more in line with the latest best practice guidelines,” says Loeb said in an NYU Langone press release. She cited a 2016 report from the American Society of Clinical Oncology, which discourages aggressive therapy for low-grade tumors.
About that time, widespread use of blood testing for prostate specific antigen (PSA) was being criticized for overdiagnosing of prostate cancer, leading to potentially harmful treatment of even small, nonaggressive tumors.
Deciding to seek treatment is not always unfavorable, Loeb pointed out, noting that issues such as infection after the initial biopsy might push men toward more active therapy. Instead, she promoted the idea of shared decision-making, where patients and physicians weigh risks and benefits together.
“The main conclusion to be drawn from the data is that if so many veterans can quickly adopt this less risky disease-management strategy, then so too might other American men if they understood the potential benefits of this option,” Loeb added.
The study emphasized that, of the 48% of veterans receiving conservative management, 30% opted for watchful waiting, while only 18% received active surveillance.
In an effort to understand why the difference, some of the same researchers sought to learn what information patients and providers need to opt for active surveillance for prostate cancer. A study in the journal Patients Education & Counseling described how the researchers conducted seven focus groups with 37 active surveillance patients in two urban clinical settings, as well as 24 semi-structured interviews with a national sample of providers.2
Study authors were able to identify six themes related to informational needs during active surveillance:
- more information on prostate cancer, including biopsy features and prognosis,
- more information on active surveillance as opposed to watchful waiting or a testing protocol,
- more information on alternative management options, including complementary medicine and lifestyle modification,
- a greater variety of informational resources, including multiple formats designed to target difference audiences,
- more social support and interaction with healthcare providers, and
- verified integrity of information, with evidence that it is trusted, multidisciplinary and secure.
“Patients and providers described numerous drawbacks to existing prostate cancer resources and a variety of unmet needs including information on prognosis, [active surveillance] testing protocols, and lifestyle modification,” the researchers concluded. “They also expressed a need for different types of resources, including interaction and unbiased information.”
The study noted the rates of conservative management are higher than prior U.S. studies in different healthcare settings, noting that in the Surveillance, Epidemiology, and End Results (SEER)–Medicare–linked database from 2010-2011, only 32% of suitable patients received conservative management. On the other hand, in some other countries, such as Sweden, 74% of low-risk patients underwent active surveillance in 2014, the article pointed out.
Study authors added that, while the VA is generally doing very well with conservative management for prostate cancer, some regional variation leaves additional room for improvement.
1. Loeb S, Byrne N, Makarov DV, Lepor H, Walter D. Use of Conservative Management for Low-Risk Prostate Cancer in the Veterans Affairs Integrated Health Care System From 2005-2015. JAMA. 2018 Jun 5;319(21):2231-2233. doi: 10.1001/jama.2018.5616. PubMed PMID: 29800017.
2. Loeb S, Curnyn C, Fagerlin A, Braithwaite RS, Schwartz MD, Lepor H, Carter HB, Ciprut S, Sedlander E. Informational needs during active surveillance for prostate cancer: A qualitative study. Patient Educ Couns. 2018 Feb;101(2):241-247. doi: 10.1016/j.pec.2017.08.022. Epub 2017 Sep 1. PubMed PMID: 28886974; PubMed Central PMCID: PMC5808852.

