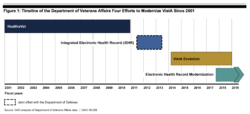
WASHINGTON—Plans are moving ahead for VA’s 10-year, $16 billion effort to modernize its electronic health record system, but legislators still have questions about the project’s timeline and funding, as well as concerns about the project’s chain of command.
Legislators expressed fear that, without a person or group at the top with final decision-making power, DoD will “roll over” VA during any major dispute regarding the system’s implementation. Those concerns were raised last month at a Senate Appropriations Committee hearing.
VA announced last May that it had signed a contract with the health technology company Cerner, the same company that had been contracted to overhaul the DoD’s electronic health record system. By adopting the same platform as DoD, VA stated that the result would be the long-sought seamless sharing of records between the two agencies, as well as an increased ability to share records with community providers, and overall improvements in efficiency and transparency.
While there exists a VA/DoD Interagency Program Office that ostensibly acts as a single point of accountability, a Government Accountability Office report in November noted that the IPO does not have decision-making authority and is not effectively positioned to act as a final arbiter.
“We’ve known since the Cerner [contract signing] in May that this process will be impossible without an entity at the top of the food chain to make decisions,” declared Sen. Jon Tester (D-MT) at the hearing. “Meantime, important decisions are being made without formal interagency structure. And some decisions are getting kicked down the road because there’s no one to make them.”
VA’s Acting Deputy Secretary John Byrne noted that the IPO is in place and working, but that, on an operational level, he and his counterpart at DoD act as the arbiters between any disagreements between DoD and VA. He admitted that it’s not a perfect process and that he would prefer an alternative.
“All of us have agreed that we would like to consider the option to have one arbitrator—a purple person whom we all agree would handle any disputes,” he said. “A ‘purple person’ is somebody not from VA or DoD.”
Tiger Team
A DoD/VA Tiger Team has been tasked with determining whether this, or some other kind of arrangement, would be a better solution in the long-term, and Byrne expected their report at the end of February. In the meantime, no effort has been made to formally reach out to anyone who might take on this ‘purple person’ role.
“We’re still seeking names and looking for that person right now,” Byrne told Tester. “If that’s the construct we decide on going forward.”
Tester remained concerned that, in the absence of this individual, VA could get “steamrolled” by DoD. “They’ve been down the road, so I think they can say ‘We have more experience than you.’”
Concerns also remain that the 10-year timeline for the full EHR rollout will leave some facilities waiting too long for much-needed interoperability. Of particular concern is the scheduling component of the EHR, which legislators predict will become increasingly necessary when new community care access standards go into effect this summer.
“In regard to scheduling, 10 years is too long,” Committee Chair Sen. John Boozman (R-AR) told VA officials. “One of the things we’re being told by VA is that efficiencies in the VA system will help pay for [increased community care access]. The critical way you do that is through scheduling. We simply have to have those efficiencies and we have to have them in a timely fashion for the mission to work and for it to be affordable.”
Byrne assured Boozman that the scheduling component would reach VA hospitals before the full EHR package roll-out is finally completed in 2030. While he would not commit to a specific timeframe for when the scheduling component would be available in all VA facilities, he did say that it would be closer to five years than 10.
The adoption of a Cerner-developed scheduling software meant the cancelling of its Medical Appointment Scheduling System (MASS) designed by Epic, a Wisconsin-based software company. The system had already gone live as a pilot project in Columbus, OH, and received early praise.
“The results of the pilot showed 30% improvement in primary care wait times, 18% improvement in behavioral health wait times; and in a 30-50% reduction in the time required to schedule an appointment,” Sen. Tammy Baldwin (D-WI) noted at the hearing. She questioned why a pilot program that showed tremendous promise should be cancelled in favor of Cerner, and was skeptical of VA’s claims that the Cerner-created scheduling software module could provide definitive streamlining at VA facilities, when it has yet to be tested in any VA facilities.
The first VA sites using the Cerner-created EHR will be pilot sites in the Pacific Northwest, which will go live in March 2020.