SEATTLE — Since the launch of the Opioid Safety Initiative in 2012, the VA has implemented a number of steps designed to reduce the use of opioids and the risk of addiction and overdose among veterans. The initiative resulted in a 41% decline in opioid prescription rates in the past five years.
Benzodiazepines, another class of highly-addictive drugs, are receiving more attention from VA researchers and policymakers, both for stand-alone prescriptions and those written for patients also prescribed opioids.
Nationwide, the number of benzodiazepine prescriptions rose 67% from 1996 to 2013, and the amount prescribed tripled. Those increases contributed to a more than sevenfold increase in overdose deaths involving the drug, from 1,135 in 1999 to 8,791 in 2015, according to a recent article in the New England Journal of Medicine co-authored by Keith Humphreys, PhD, of the Veterans Affairs Palo Alto Health Care System and the Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine.1
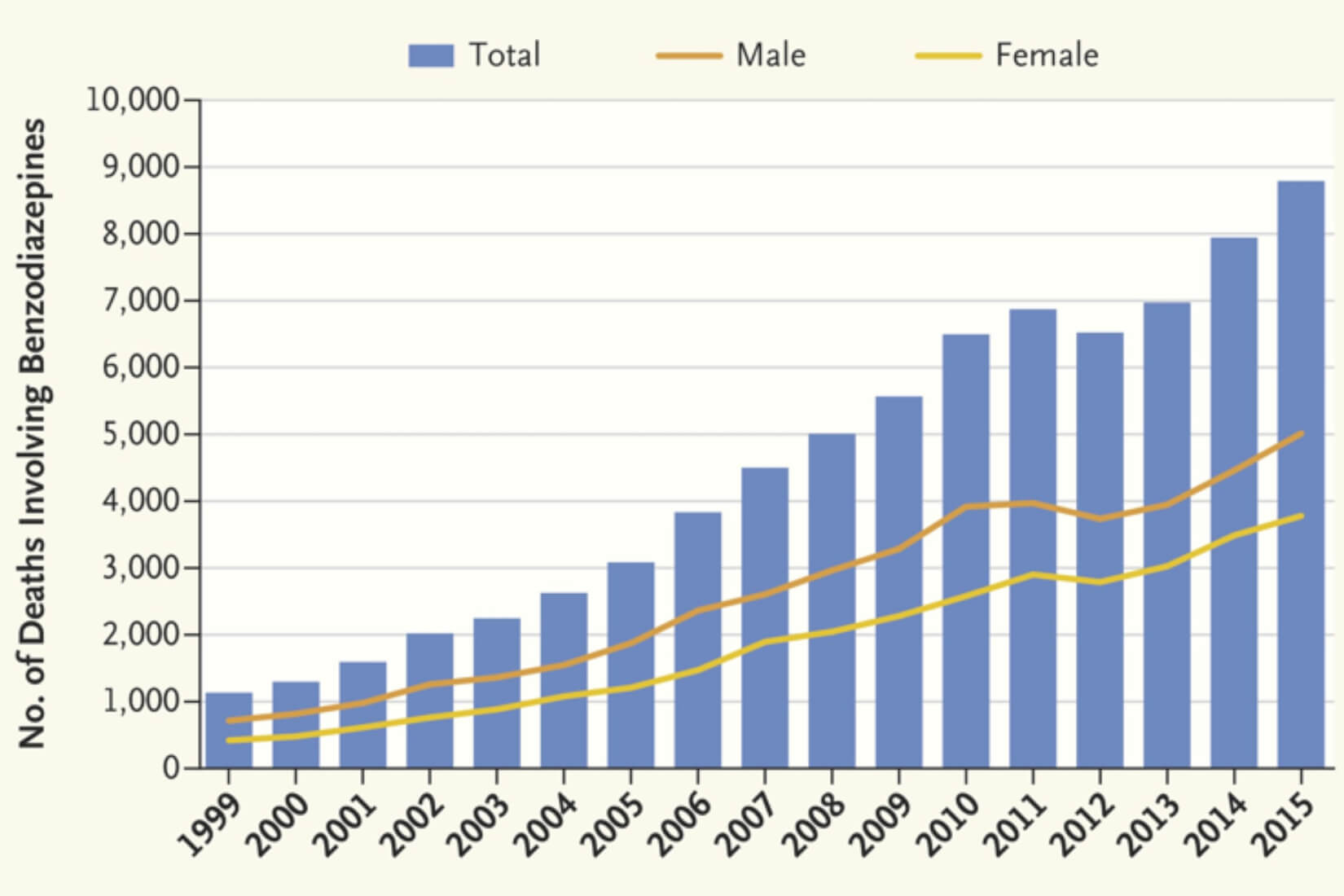
From the National Institute on Drug Abuse
Only opioids are associated with more deaths from overdoses than benzodiazepines, and the overdose risk rises almost 400% for individuals who take both types of drugs. Nearly half of the 2,400 veterans who died of opioid overdoses between 2004 and 2009 had a concurrent benzodiazepine prescription. Veterans with any history of benzodiazepine prescriptions had twice the risk of those with no such history and the higher the dose of benzodiazepine, the greater the overdose risk.2
Overall, 27% of veterans who receive care through the VA and who have an opioid prescription also have one for a benzodiazepine.
Many veterans receive benzodiazepine prescriptions to address symptoms of post-traumatic stress disorder (PTSD),even though the VA has strongly recommended against prescribing benzodiazepines for the disorder since 2010. Multiple randomized clinical trials have found the medications ineffective for long-term treatment of PTSD, and they appear to reduce response to psychotherapy and worsen symptoms.
When used, benzodiazepines should be prescribed for a month or less because of the high risk of dependence, which develops in many patients after only four to six weeks, according to the VA brochure, Re-evaluating the Use of Benzodiazepines. “Many prescribers don’t realize that benzodiazepines can be addictive and when taken daily can worsen anxiety, contribute to persistent insomnia, and cause death,” noted Humphreys and his colleagues.
Benzodiazepines also increase the risk of memory issues, dementia, cognitive impairment, depression, emotional lability, aggressive behavior, car accidents, falls, birth defects and fatigue. They may worsen symptoms of PTSD, chronic obstructive pulmonary disease and sleep apnea, and have a rebound effect in other conditions for which they are commonly prescribed, according to VA materials.
As with opioids, the VA recommends that clinicians “do not initiate benzodiazepines. If benzodiazepines are started, a clearly defined exit plan should be determined and then communicated to the veteran.” The VA’s Pharmacy Benefits Management Academic Detailing Service created tools for clinicians and patients to increase understanding of risks associated with benzodiazepines and safely discontinue their use in those who have had long-term prescriptions.
Co-prescribing Alert
In conjunction with Pharmacy Benefits Management, investigators at the VA Puget Sound Health Care System developed a point-of-prescribing alert that warned providers when opioids or benzodiazepines were prescribed to particularly high-risk patients who already had a prescription for the other drug class. The alert included the reasons a patient was considered high risk, whether because of a diagnosis, recent hospitalization or other factor.
“We were very aware going into this project that the combination of opioids and benzodiazepines can make for a dangerous combination—especially for high-risk patients with substance use disorder, sleep apnea and suicide risk,” said lead investigator Eric J. Hawkins, PhD, associate director of the VA Seattle Center of Excellence in Substance Abuse Treatment and Education and an assistant professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington in Seattle.
The alert also flagged co-prescribing in veterans aged 65 or older. It did not warn providers of every occurrence of co-prescription of the two drug classes to prevent alert fatigue, the authors said.
A recently published study found that 100 primary care providers and 53 mental health providers received alerts for a total of 1,332 patients during the initiative’s first year of implementation. One in four patients fell in more than one of the high-risk groups.
During the six months preceding the first alert, 66% of veterans had filled an opioid prescription for 90 days or more, while 60% had filled a benzodiazepine prescription for at least 90 days.
“This alert did lead to consistent, modest reductions among patients who were the most vulnerable to harm, and the alert complemented the VA’s ongoing efforts to address the opioid crisis,” Hawkins told U.S. Medicine.
Co-prescribing dropped 25% for patients with a substance use disorder diagnosis and 39% for veterans with sleep apnea. Patients at risk for suicide saw the greatest change in prescription practices, with a decline of 69% in co-prescribing.
The rate of concurrent opioid and benzodiazepine prescriptions among patients 65 and older did not change, however. Despite the reductions seen, nearly 70% of patients who had long-term prescriptions for both drug classes at the start of the study continued to concurrently fill prescriptions for benzodiazepines and opioids six months after the system first alerted their providers.
When the researchers compared the results at the Puget Sound VA to that of a similarly sized VA system that did not implement the alert, they found Puget Sound had a greater decline in co-prescribing and “greater decreases in benzodiazepine prescribing in the substance use disorder cohort and the sleep apnea cohort at VA Puget Sound” compared to the other site, Hawkins said. The researchers did not see differences between the two systems in opioid prescribing for any of the cohorts.
The alert is available nationally through Pharmacy Benefits Management. Eight other VA facilities have implemented it in the last two years, according to Hawkins.
1Lembke A, Papac J, Humphreys K. Our Other Prescription Drug Problem. N Engl J Med. 2018 Feb 22;378(8):693-695.
2Park TW, Saitz R, Ganoczy D, Ilgen MA, Bohnert AS. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ. 2015 Jun 10;350:h2698.
3Soyka M. Treatment of Benzodiazepine Dependence. N Engl J Med. 2017 Mar 23;376(12):1147-1157.
4Malte CA, Berger D, Saxon AJ, Hagedorn HJ, Achtmeyer CE, Mariano AJ, Hawkins EJ. Electronic Medical Record Alert Associated With Reduced Opioid and Benzodiazepine Coprescribing in High-risk Veteran Patients. Med Care. 2018 Feb;56(2):171-178.