Extended Prescribing Dropped from 9.5% in 2012 to 6.2% in 2016
By Brenda L. Mooney
IOWA CITY, IA—Long-term prescribing of opioid painkillers is on the decline at the VA, in contrast to what appears to be happening outside of federal medicine.
A new study in the Journal of General Internal Medicine reports that overall opioid prescribing has fallen from a peak in 2012, primarily because of long-term prescribing has dropped. Study authors led by Katherine Hadlandsmyth, PhD, of the Iowa City, IA, VA Healthcare System and the University of Iowa pointed out that longer-term opioid use creates much more opportunity for harmful side effects, compared with short-term use.1
Study authors also emphasized that studies of healthcare in the United States outside of the VHA demonstrate decreases in short-term opioid prescriptions but not long-term ones.
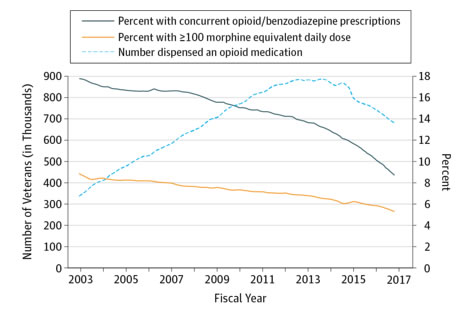
Veterans Dispensed at Least 1 Opioid Medication in the VA Health Care System and Percent of Opioid Recipients With Concurrent Benzodiazepine Prescriptions and High Opioid DosageData are from VA Pharmacy Benefits Management Services and presented by quarter, fiscal years 2003 through 2016.
Hadlandsmyth suggested that other healthcare systems could learn from the VHA example, adding, “Future work to understand precisely which initiatives have most positively impacted opioid prescribing would be necessary to maintain effective approaches within VHA.” See related Pharmacy Update, p. xx
For the study, researchers analyzed VHA prescription data from 2010 to 2016, which included more than four million veterans per year. They found that, in 2010, opioids were prescribed at least once to 20.8%—962,193 out of around 4.63 million—VA patients. Six years later, the percentage had declined to 16.1, representing 803,888 of 4.99 million veterans who received outpatient prescriptions for opioid products such as hydrocodone, oxycodone and fentanyl.
Drilling down into the results, study authors found that long-term use accounted for about 90% of VHA opioid prescriptions during the study period. That decreased, however, from 9.5% in 2012, to 6.2% in 2016.
Hadlandsmyth suggested that was not because many existing long-term users stopped taking opioids but because fewer veterans receiving new opioid prescriptions ultimately became long-term opioid users. The data backed her up, with the likelihood of a veteran becoming a new long-term opioid user falling overall from 2.8% in 2011 to 1.1% in 2016.
“The prevalence of opioid prescribing was 20.8% in 2010, peaked at 21.2% in 2012, and declined annually to 16.1% in 2016,” the researchers wrote. “Between 2010 and 2016, reductions in long-term opioid prescribing accounted for 83% of the overall decline in opioid prescription fills. Comparing data from 2010-2011 to data from 2015-2016, declining rates in new long-term use accounted for more than 90% of the decreasing prevalence of long-term opioid use in the VHA, whereas increases in cessation among existing long-term users accounted for less than 10%. The relative risk of transitioning to long-term use during 2016 was 6.5 (95% CI: 6.4, 6.7) among short-term users and 35.5 (95% CI: 34.8, 36.3) among intermediate users, relative to patients with no opioid prescriptions filled during 2015.”
VHA Initiatives
Hadlandsmyth credited recent initiatives by the VHA with improving prescribing patterns; those programs emphasize opioid safety and nonopioid alternatives for chronic pain treatment. Since 2010, VHA has provided clinical practice guidelines to medical practitioners about how best to use opioids to manage chronic pain and how to select and monitor patients. These guidelines also include suggestions on how to wean patients off opioid medications, if treatment goals are not reached.
In late 2013, VHA launched the Opioid Safety Initiative (OSI) to promote safer opioid prescribing. The OSI employs an “audit and feedback” model, which has been used successfully in other efforts to improve healthcare quality and safety. Because the national VA system uses a single computerized electronic medical record system, it was a good candidate for the dashboard approach so that each hospital’s OSI “champion” could easily see how opioids and related medications were being prescribed at their hospital and by each doctor who prescribed them. That information could then be compared with national and regional data.
In addition to the previous guidelines and the dashboard, the opioid initiative encouraged local hospital leaders to provide education about pain care and opioid prescribing. At the same time, the data and tools could be tailored to individual patient needs. An issue in reducing the use of high-dose opioids is that changing the dose must be done gradually and carefully, especially when a patient has been accustomed to higher doses over a longer period of time, according to the VHA’s practice guidance.
Hadlandsmyth pointed out that VHA now also regularly considers complementary treatments and multimodal therapy options for pain management, including behavioral, chiropractic and stepped care. With the MHS, VA had become among the most-active large healthcare systems in the United States in use of complementary and alternative therapies, primarily for pain management and mental health issues.
“Opioid prescribing trends followed similar trajectories in VHA and non-VHA settings, peaking around 2012 and subsequently declining. However, changes in long-term opioid prescribing accounted for most of the decline in the VHA,” the study authors concluded. “Recent VA opioid initiatives may be preventing patients from initiating long-term use. This may offer valuable lessons generalizable to other healthcare systems.”
A University of Maryland study also looked at longer-term patterns of opioid prescribing in the VHA as a way to determine the effects of the educational campaigns introduced in 2010 and 2013.
For the report in the November/December 2017 issue of the Journal of Addiction Medicine, researchers created a national cohort that documents more than 21 million patient records and 97 million outpatient opioid pain management (OPM) prescriptions covering a 17-year period. Prescribing in emergency departments, outpatient clinics, and inpatient settings was included in the data.2
Reviewed were 2.5 billion outpatient clinic visits, 18.9 million emergency department visits and 12.4 million hospital admissions, with results showing that the number of OPM prescriptions peaked in 2011. At that time, the narcotic painkillers were provided during 5% of all outpatient visits and 15% of all emergency department visits.
At the same time, the morphine milligram equivalents (MMEs) peaked in 2014 at almost 17 billion in outpatient clinics and at 137 million in emergency departments.
In contrast, by 2016, OPM prescriptions were down 37% in outpatient clinics and 23% in EDs, and MMEs were down 30% in both settings.
The trend was not straight downward, however. The study noted that prescriptions for hydrocodone and tramadol increased substantially between 2011 and 2015, and that OPM doses in inpatient settings continued their rise until 2015.
“We used a large national cohort to study trends in OPM prescriptions within the VA. Educational efforts to reduce the number of OPM prescriptions coincided with these reductions but were initially associated with an increase in OPM dosage, an increase in the use of tramadol and hydrocodone and an increase in the use of OPMs in inpatient settings,” the study authors wrote.
A Viewpoint article published this past spring in JAMA Internal Medicine included VA officials’ take on their success in reducing opioid prescriptions. Among the authors were now-VA Secretary David Shulkin, MD, lead author Wallad F. Gellad, MD, MPH of the Center for Health Equity Research and Promotion and co-author Chester B. Good, MD, MPH, of the Center for Pharmaceutical Policy and Prescribing, both at the VA Pittsburgh Healthcare System.3
The article pointed out that VA has some advantages over other healthcare providers in addressing issues such as opioid over-prescribing. Among them:
- VA’s integrated financing and delivery system allows it to institute uniform policies without regard to reimbursement;
- The VA has full data capture across the spectrum of health services, including outpatient, inpatient, pharmacy and rehabilitation.
Pharmacists have a larger role and scope of practice at the VA to manage the opioid epidemic, from promoting naloxone use to recommending alternative pain medications.
“Although the VA has made progress, important lessons have also been learned,” the authors recounted. “First, efforts to effectively manage pain while decreasing opioid use may pose challenges for individual patients. Some clinicians may become reluctant to prescribe opioids in situations when they are indicated, or may inappropriately strive to get patients under specific dosages to achieve performance metrics. In response to limitations on prescription opioids, some patients may obtain medications from other healthcare systems or illegally. The balance between appropriately treating pain and reducing the risks of opioid use requires careful attention. Importantly, the focus is on reducing opioid risks—in some cases this means reducing the number of patients receiving opioids, but in other cases it means improving the safety of opioid use among those who require such medications”.
The viewpoint article described how the VA has struggled to uncover better methods of both managing pain in veterans and limiting the risks of opioids. “In 2017, fewer veterans are receiving high doses of opioids or concomitant interacting medicines like benzodiazepines, and more veterans are receiving nonopioid pain therapies, naloxone, and treatment for substance use disorders,” the Viewpoint authors wrote. “The VA provides an example of how technology, data, and organizational leadership can make a difference in improving opioid prescribing.”
1. Hadlandsmyth K, Mosher H, Vander Weg MW, Lund BC. Decline in PrescriptionOpioids Attributable to Decreases in Long-Term Use: A Retrospective Study in the Veterans’ Health Administration 2010-2016. J Gen Intern Med. 2018 Jan 29. doi:10.1007/s11606-017-4283-8. [Epub ahead of print] PubMed PMID: 29380212.
- Grasso MA, Grasso CT, Jerrard DA. Prescriptions Written for Opioid Pain Medication in the Veterans Health Administration Between 2000 and 2016. J Addict Med. 2017 Nov/Dec;11(6):483-488. doi: 10.1097/ADM.0000000000000352. PubMed PMID:
28858889.
- Gellad WF, Good CB, Shulkin DJ. Addressing the Opioid Epidemic in the United States: Lessons From the Department of Veterans Affairs. JAMA Intern Med. 2017 May 1;177(5):611-612. doi: 10.1001/jamainternmed.2017.0147. PubMed PMID: 28288245.
