BIRMINGHAM, AL—Even more than other veterans, those in rural areas often see providers and obtain medications outside the VA system, in many cases because the closest VA facility might be distant from their home or they have a primary care provider in their community.
That likely is even more the case with the Veterans CHOICE Act expanding community access for veterans. One result is the critical need to obtain medication information from outside sources to create a best possible medication history for these patients.
A study in the American Journal of Health System Pharmacy noted that high-quality medication reconciliation reduces medication discrepancies, but limited resources sometimes makes it difficult for smaller hospitals to do that. The authors said they sought to adapt and implement an evidence-based toolkit of best practices for medication reconciliation in smaller hospitals, evaluate the effect on unintentional medication discrepancies, and assess facilitators and barriers to implementation.1
As part of the approach, the University of Alabama at Birmingham researchers and colleagues conducted a two-year mentored-implementation quality improvement feasibility study in three VA hospitals serving rural patients. The study team—including participation from the Center for Applied Systems Engineering, VISN11-Veterans Engineering Resource Center, in Indianapolis; the Iowa City VA Healthcare System in Iowa City, IA, and the VA Tennessee Valley Healthcare System, in Nashville, as well as Vanderbilt and Harvard universities—designated unintentional medication discrepancies per medication per patient as the primary outcome, determining that by comparing the “gold standard” preadmission medication history to the documented preadmission medication list and admission and discharge orders.
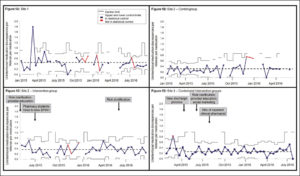
Included were 797 patients, with an average age of 68.7 years; the 94.4% male participants were prescribed an average of 9.6 medications. Two of the three sites implemented toolkit interventions, including clarifying roles among clinical personnel, educating providers on taking a best possible medication history and hiring pharmacy professionals to obtain a best possible medication history and perform discharge medication reconciliation. At one of the two sites with toolkit intervention, discrepancies improved in intervention patients compared with controls (adjusted incidence rate ratio [IRR], 0.55; 95% confidence interval [CI], 0.45–0.67) but that was not the case at the other site (adjusted IRR, 1.22; 95% CI, 1.08-1.36).
“An evidence-based toolkit for medication reconciliation adapted to the VA setting was adopted in two of three small, rural, resource-limited hospitals, resulting in both reduced and increased unintentional medication discrepancies. We highlight facilitators and barriers to implementing evidence-based medication reconciliation in smaller hospitals,” the authors concluded.
The Rural VA Multi-Center Medication Reconciliation Quality Improvement Study (R-VA-MARQUIS) “demonstrates that an evidence-based toolkit of best practices for medication reconciliation can be deployed in smaller, resource-limited facilities, including those serving rural patients who have limited access to clinical pharmacy services. Institutional and senior leadership support are critical to successful implementation. Competency assessments for BPMH education and monitoring of intervention fidelity are integral to intervention effectiveness in medication reconciliation improvement work. Reconciling medications at discharge, with allocation of resources to high-risk patients, may also be important for success. These results highlight the need for additional study within the VA and smaller hospitals serving rural populations. Results and experience gleaned from R-VA-MARQUIS have informed the VA’s national medication reconciliation policy and tools, including a VA-wide effort to standardize and improve medication reconciliation.”
Medication reconciliation, the process of identifying and providing the most accurate medications for a patient anywhere in the healthcare system to resolve medication discrepancies and prevent adverse drug effects, is required by the Joint Commission at all transitions of care across all sites of care. Recognizing that significant variation in the quality of medication reconciliation persists, the VA started the Medication Reconciliation Initiative in 2008. The national program tracks compliance with medication reconciliation requirements and requires VA facilities to align their medication reconciliation practices to meet both Joint Commission and internal requirements. The authors pointed out, however, that implementing evidence-based best practices for inpatient medication reconciliation has been difficult to initiate and sustain across healthcare systems.
The Multi-Center Medication Reconciliation Quality Improvement Study, conducted from 2011-2014, used a mentored-implementation approach to test an evidence-based toolkit of best practices for inpatient medication reconciliation at five hospitals, including one in the VA system, reducing unintentional medication discrepancies by 8% a month.2
Background information in the report noted that patients are vulnerable to adverse drug events due to medications, especially during care transitions. ADEs occur in 5% to 40% of hospitalized patients and 11% to 19% of patients after discharge, according to the authors, and unintentional medication discrepancies or unexplained differences in medication regimens across sites of care, are associated with ADEs.
Furthermore, they wrote, discrepancies are documented in 67% of patients at admission and 40% of patients at discharge, with patients taking more than five medications at increased risk for medication discrepancies. The article cited a VA study indicating that 60% of veterans were found to have one or more medication discrepancy In addition, veterans living in rural areas were less likely to use clinical pharmacy services than those living in urban areas, contributing to a higher risk of discrepancies and ADEs.3
“Our study had results comparable to those of the original MARQUIS, the largest mentored-implementation study of best practices for medication reconciliation. In MARQUIS, four of five sites implemented toolkit interventions; three sites reduced potentially harmful unintentional medication discrepancies,” researchers explained. “Although our primary outcome was unintentional medication discrepancies, these are known to correlate with potentially harmful discrepancies”
The authors added, “Prior studies have shown that pharmacy-driven medication reconciliation processes and patient counseling at discharge can reduce unintentional medication discrepancies and preventable ADEs. Site 3’s reduction in unintentional medication discrepancies after hiring an inpatient clinical pharmacist and implementing a pharmacy-driven discharge-medication reconciliation and counseling process reinforces the importance of this type of intervention.”
The report suggested that different results at Site 2 might have been related to too little pharmacist supervision.
“The factors contributing to successful implementation—institutional and senior leadership support, alignment with institutional priorities, physician engagement, teamwork, interdisciplinary coordination and emphasis on patient safety—are similar to previously reported facilitators. The common barriers to implementation are echoed in a prior mentored-implementation study, including time constraints of staff and perceived lower priority of the project institutionally,” the authors wrote. “If the toolkit is adopted by hospitals with large rural populations, future iterations must address the specific issues in caring for rural patients including the need for greater coordination at discharge to accommodate travel and to gather medication information from outside sources.”
- Presley CA, Wooldridge KT, Byerly SH, et al. The Rural VA Multi-Center Medication Reconciliation Quality Improvement Study (R-VA-MARQUIS). Am J Health Syst Pharm. 2020;77(2):128-137. doi:10.1093/ajhp/zxz275.
- Schnipper JL, Mixon A, Stein J, et al. Effects of a multifaceted medication reconciliation quality improvement intervention on patient safety: final results of the MARQUIS study. BMJ Qual Saf. 2018;27(12):954-964. doi:10.1136/bmjqs-2018-008233.
- Linsky A, Simon SR. Medication discrepancies in integrated electronic health records. BMJ Qual Saf.2013; 22:103-9.