 BUFFALO, NY – While reports in the literature are increasing about high rates of coagulopathy and venous thromboembolism (VTE) among hospitalized patients with coronavirus disease 2019 (COVID-19), there is little guidance on how to treat it or prevent it.
BUFFALO, NY – While reports in the literature are increasing about high rates of coagulopathy and venous thromboembolism (VTE) among hospitalized patients with coronavirus disease 2019 (COVID-19), there is little guidance on how to treat it or prevent it.
“Understanding of these abnormalities is continually evolving, but these conditions may pose a risk to COVID-19 patients beyond the risk typically seen in critically ill patients,” advised authors from the VA Western New York Healthcare System in Buffalo and colleagues.
Their article in the American Journal of Health System Pharmacy pointed out that no widely accepted evidence-based guidelines are available for specifics related to treatment and prevention of COVID-19-related coagulopathies.1
Among those management issues were:
-
Agent selection and dosing,
-
Continuation vs interruption of home oral anticoagulant therapy during hospital admission, and
-
Post-discharge VTE prophylaxis.
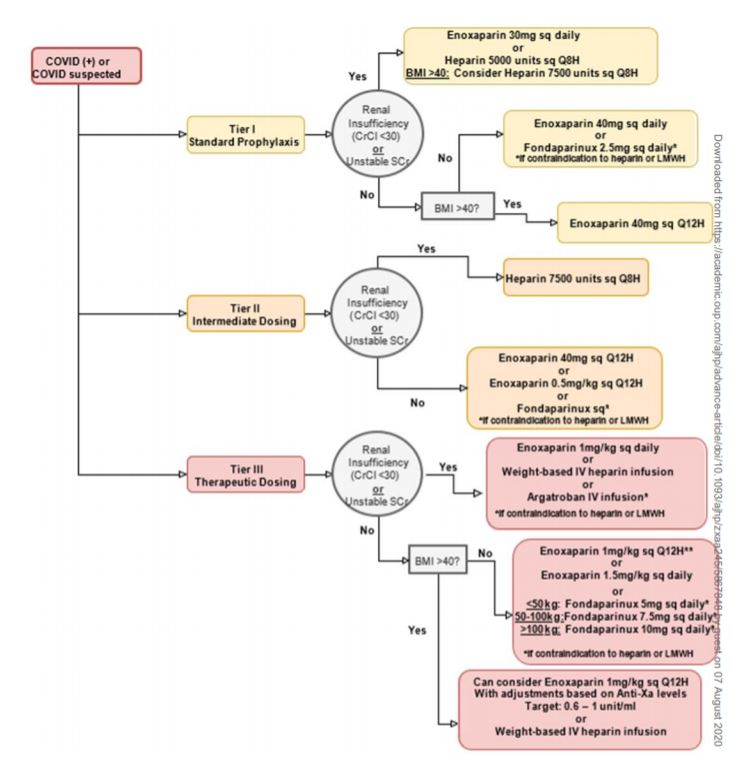
“Clinicians may wish to consider use of a stratified, 3-tiered approach of low-intensity anticoagulation, intermediate-intensity anticoagulation, and therapeutic-dose anticoagulation. Patients can be categorized by tier depending on their risk factors for VTE, acuity of illness, and laboratory values such as D-dimer level,” according to the article.
The authors said they are offering guidance on anticoagulation consideration and dosing “to assist clinicians faced with challenging anticoagulation-related situations in caring for hospitalized COVID patients until formal evidence-based guidelines become available.”
The review noted that hematologic abnormalities commonly seen in patients with COVID-19 include elevations in D-dimer and fibrinogen, prolonged prothrombin time and activated partial thromboplastin time (aPTT), as well as changes in levels of inflammatory markers such as C-reactive protein (CRP), interleukin-6, and ferritin.
“Understanding of these abnormalities is continually evolving, but they may pose a risk to patients with COVID-19 beyond the risk typically seen in critically ill patients,” the authors wrote, pointing out that abnormalities in coagulation markers might signal greater disease severity and that higher D-dimer levels are associated with increased mortality.
The pharmacist team also called it “an encouraging sign for treatment of patients with COVID-19” that available anticoagulants have shown some benefit.
“There are increasing reports in the literature of high rates of coagulopathy and venous thromboembolism (VTE) among hospitalized patients with coronavirus disease 2019 (COVID19). 1-5 Hematologic abnormalities commonly seen in patients with COVID-19 include elevations in D-dimer and fibrinogen, prolonged prothrombin time and activated partial thromboplastin time (aPTT), and changes in levels of inflammatory markers such as C-reactive protein (CRP), interleukin-6, and ferritin,” the authors explained. “Understanding of these abnormalities is continually evolving, but they may pose a risk to patients with COVID-19 beyond the risk typically seen in critically ill patients.”
Earlier studies have reported that abnormalities in coagulation markers are indicators of disease severity and that higher D-dimer levels are associated with increased mortality. Other researcher has suggested that those experiencing VTE were more likely to be older and to have prolonged aPTT and elevated D-dimer levels and that the incidence of thrombotic complications has been reported to be 20% to 31% in critically ill patients with COVID-19 despite use of standard VTE prophylaxis.
The article also discussed post–hospital discharge VTE prophylaxis, stating that it “represents another area of clinical uncertainly that will require a careful weighing of the risks vs potential benefits of ongoing therapy.”
“We suggest that upon discharge all patients, regardless of tier, be assessed for ongoing need for continued prophylaxis. Careful examination of additional risk factors for VTE, such as prolonged immobility while in quarantine, as well as trends in laboratory values, such as D-dimer, CRP, ferritin, and lactate dehydrogenase levels, should be reviewed,” according to the study. “Elevated inflammatory markers may indicate an increased risk of VTE upon a patient’s discharge to home, and continued prophylaxis may be warranted. In the absence of randomized, controlled clinical trials, clinicians may wish to consider use of LMWH instead of direct-acting oral anticoagulants (DOACs) or other agents due to the former’s anti-inflammatory effects.”
They added that DOACs could be an option if compliance concerns arise, such as a patient’s unwillingness to use parenteral therapy or inability to self-inject.
The authors further advised that duration of prophylactic therapy should be determined on a case-by-case basis, taking into account bleeding risk. “Consideration of extended prophylaxis of up to 45 days may be appropriate in patients at increased risk for VTE who are at low risk for bleeding. For patients who had been using a DOAC at home and were transitioned to parenteral anticoagulation during an inpatient stay, a transition back to home DOAC therapy may be considered in the absence of evidence of treatment failure. Upon discharge of patients with confirmed or suspected VTE, continuation of anticoagulation treatment for minimum 3 months for provoked VTE can be chosen,” they wrote.
The article also suggested that treatment with therapeutic-dose LMWH or DOAC therapy can be considered in preference to warfarin, in accordance with current guidelines, adding, “If VTE is not confirmed at time of discharge due to lack of test availability, the clinician may wish to treat according to conventional protocols for VTE.”
The pharmacists authors cautioned that the situation is fluid and that their recommendations could change, explaining, “We recognize that the guidance presented in this article has significant limitations, and we hope that clinicians will benefit from a growing body of evidence-based and standardized guidelines on the issues discussed here. As with all treatment options for patients with COVID19, this is a fluid situation. The preceding is not intended as a practice management protocol; rather, the intent is to provide practical suggestions for clinicians treating this novel disease.”
- Smith K, Krajewski KC, Krajewski MP. Practical considerations in prevention and treatment of venous thromboembolism in hospitalized patients with COVID-19 [published online ahead of print, 2020 Jul 6]. Am J Health Syst Pharm. 2020;zxaa245. doi:10.1093/ajhp/zxaa245
