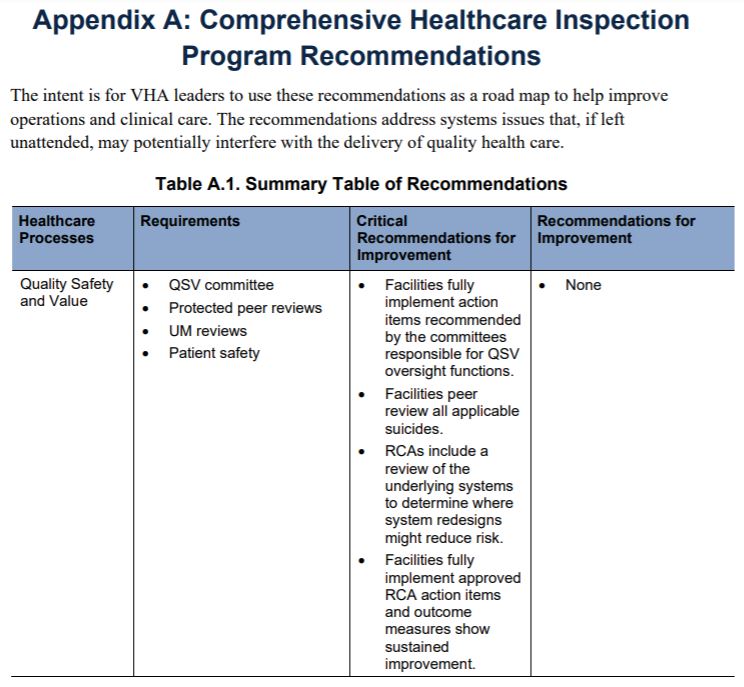
WASHINGTON, DC — The quality, safety and value (QSV) programs in some VA facilities continue to fall short, according to a new VA Inspector General report.
A document released last month pointed out that those included a failure to timely review patient deaths, to peer review suicides following patient discharges from an inpatient mental health unit, to provide regular reviews of peer review committees’ work, and to document the work of utilization management (UM) physician advisers tasked with improving healthcare safety and efficiency within hospitals. Of these, all except reviewing suicides are repeat findings from previous reports released in 2018 and 2019.
When interviewed, VA employees frequently placed the blame for these deficiencies on a lack of oversight at the leadership level coupled with inadequate staffing levels at the facility.
From November 2019 through September 2020, the OIG conducted unannounced inspections of 36 VA medical centers, interviewing staff and facility leaders with a focus on the administrative processes designed to ensure a consistent quality of care for veterans.
“The results in the report are a snapshot of VHA performance at the time of the fiscal year 2020 OIG reviews,” the report noted. “The findings in this report may help VHA identify areas or conditions that, if properly addressed, could improve patient safety and healthcare quality.”
Two of the findings centered on how facilities investigate deaths of patients, both in the hospital and immediately following their discharge. VHA requires that hospitals conduct a peer review of all patient deaths that occur within 24 hours of admission, if that death is not expected. The purpose of the review is so that facilities can determine quickly if the death was the result of improper medical procedures and, if so, to adjust those procedures before they can affect other patients. About a quarter of facilities in the OIG review had failed to complete their reviews within that initial 24 hours.
VHA also requires facilities to review all suicides that occur within seven days following a patient’s discharge from an inpatient mental health unit or residential care facility. Of the facilities that had suicides during the report’s timeframe, 13% failed to complete peer reviews.
Missed Opportunities
“This resulted in missed opportunities to identify and address potential improvement needs for clinical practice and organizational performance,” the investigators stated in their report. “Some facility managers reported lack of attention to detail and lack of oversight as reasons for noncompliance.”
Facilities were also deficient in conducting root cause analyses (RCA) of adverse events. Of the 178 RCAs that investigators reviewed, 31 did not include an analysis of the underlying systems that might have contributed to the event. The goal of that kind of analysis is to determine where system redesigns might reduce risk.
This and other deficiencies “likely limited reviews’ ability to identify vulnerabilities and resulted in inadequate implementation of process improvements that could help prevent patient harm,” the report noted.
To ensure that a facility’s peer review committee is doing its job properly, VHA requires that a summary of the committee’s work be reviewed quarterly by an executive-level medical committee. However, OIG found that 6 out of 36 facilities failed to consistently provide summaries for review. Again, the reason given was a general lack of oversight, as well as a lack of staffing.
The report also found issues with facilities’ full participation in the Utilization Management (UM) program—part of VA’s National Center for Patient Safety. The UM program is designed to provide consultation services that help facilities ensure that patients are receiving the right care at the right time. UM physicians will measure quality initiatives at facilities, review inpatient cases and provide guidance, and conduct needs-based reviews and make modifications to patient care coordination where needed.
UM physicians are also required to upload the decisions they make on at least 75% of inpatient stays to a national database. About 14% of facilities failed to do this, resulting in an “inadequate level of evaluations for the appropriateness of admissions and continued stays.”
While VA concurred with the recommendations, OIG noted that the department’s current action plans to address the issues are lacking in detail and will require regular monitoring by inspectors going forward.