No Change in Mortality Rates After Veterans’ Choice, However

In May, Cecilia M. Beauprie, chief nurse of Outpatient Nursing Service and Community Based Outpatient Clinics at the Edward Hines, Jr. VA Hospital near Chicago, presents to other nurse leaders in May. The goal was to optimize care for veterans. Photo by Louis Washkowiak, Hines VA Hospital Media Services
MENLO PARK, CA — Hospitalization within the VA healthcare system showed a modest decline, and VA-paid community hospitalization increased moderately from January 2012 to December 2017 with the implementation of the Veterans’ Choice Act of 2014 (VCA); but mortality rates appeared to be unchanged, according to a recent report.
Hospitalization at the VHA dropped 4%, while community hospitalizations of covered veterans went up 5% after the act was put into effect, according to a research letter published in JAMA Health Forum.1
“The US VA MISSION Act of 2018 further expanded the access of veterans to community care and is expected to amplify the trends observed in this study,” wrote authors from the Health Economics Resource Center at the VA Palo Alto, CA, Healthcare System,
“Better surgical outcomes were recently documented in VA hospitals compared with the private sector, so greater privatization of care for veterans may not translate to improved quality and outcomes,” the researchers advised. “Shifting inpatient care to non-VA hospitals poses substantial challenges for care coordination across clinicians and health care systems and requires that outcomes and quality of care be closely monitored.”
A study late last year found that perioperative outcomes at the VHA are consistently better than those in private sector hospitals. The report in JAMA Surgery pointed out that the national cohort study looking at more than four million surgical procedures found that surgical care provided in the VA healthcare system was associated with lower perioperative mortality and decreased failure to rescue.2
More recently, new research comparing mortality among veterans treated with emergency care at VA and non-VA hospitals is the latest in a growing number to suggest that the care received in VA hospitals compares favorably to that received in non-VA centers.3
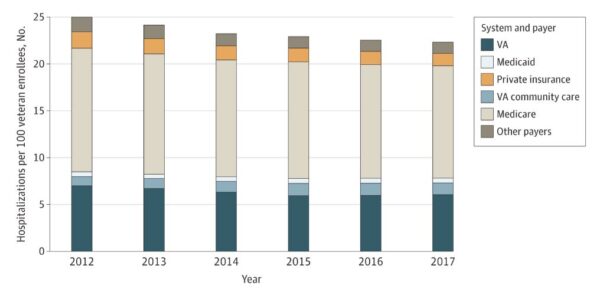
Click to Enlarge: Total Number of Hospitalizations per 100 Veterans Enrolled in the Veterans Affairs (VA) Health Care System by System and Payer From 2012 to 2017
The mortality rates are significant because advocates of community care for VA beneficiaries emphasized that veterans had died waiting for VA care and that their proposals would remedy that. While it remains somewhat unclear how many patients died during a wait list scandal centered at the VA’s Phoenix healthcare system, the numbers have ranged from 40 to 80.
Another factor in changing usage of care inside the VHA is Medicaid expansion. The authors pointed out that, although the number of Medicaid hospitalizations was small, expansion of the program was associated with a 19% increase in community hospitalizations of veterans and a 2.5% decrease in VA hospitalizations. Again, no change in mortality was identified.
“Veterans enrolled in the Veterans Affairs (VA) health care system have access to non-VA care through VA community care programs or other health insurance coverage,” the study noted. “Access has increased in recent years because of the expansion of Medicaid programs under the Affordable Care Act and the US Veterans’ Choice Act (VCA), which increased VA-paid community care.”
Five States
The research team sought to determine the association between those policies and utilization and outcomes. To do that, it conducted a longitudinal study with repeated cross-sections of veterans for a total of 13 million veteran-years in five diverse states—Arizona, California, Florida, New York and Pennsylvania—from 2012 to 2017.
The effort linked VA enrollment records, VA acute hospital records and all-payer hospital discharge data for a comprehensive set of hospitalization records for veteran beneficiaries. Demographic information was compiled on age, sex, race and ethnicity [self-reported], marital status, VA enrollment category and state. At the same time, VA administrative data was used to establish the date of death, the number of hospitalizations by system and payer from VA and state discharge data.
Separate models were used to examine changes occurring after Medicaid expansion by state and year and the post-VCA period beginning with 2015, the first full year of implementation.
Results indicated that, during the six-year period, the number of VA enrollees in the five states grew from 2.2 to 2.4 million. While the mean age (61-62 years) and the percentage of men (92%-94%) were similar, the percentage of enrollees with military service–connected disabilities increased from 24% to 33%.
Overall, the study identified fewer total hospitalizations among enrollees, with the mean number of VA acute hospitalizations declining 14%. At the same time, the mean number of VA-paid community hospitalizations grew 26%.
Medicare covered more hospitalizations (54%) than any other payer, while Medicaid covered only 2% of hospitalizations throughout the study period.
“To our knowledge, this is the first study since the VCA and Medicaid expansion to examine changes in hospitalizations while using all-payer hospital data,” researchers pointed out. “Veterans increased use of community hospitals paid by VA and Medicaid and decreased use of VA hospitals when access to non-VA care expanded. This shift in hospitalizations to the community was not associated with changes in mortality, although other outcomes need to be assessed to understand how changes in hospital utilization were associated with quality of care.”
The authors noted that, while the hospitalizations of most veterans were covered by Medicare in some cases, a lot of veterans continued to rely on VA hospitals.
- Yoon J, Kizer KW, Ong MK, et al. Health Care Access Expansions and Use of Veterans Affairs and Other Hospitals by Veterans. JAMA Health Forum. 2022;3(6):e221409. doi:10.1001/jamahealthforum.2022.1409
- George EL, Massarweh NN, Youk A, et al. Comparing Veterans Affairs and Private Sector Perioperative Outcomes After Noncardiac Surgery. JAMA Surg. Published online December 29, 2021. doi:10.1001/jamasurg.2021.6488
- Chan DC, Danesh K, Costantini S, Card D, Taylor L, Studdert DM. Mortality among US veterans after emergency visits to Veterans Affairs and other hospitals: retrospective cohort study. BMJ. 2022 Feb 16;376:e068099. doi: 10.1136/bmj-2021-068099. PMID: 35173019; PMCID: PMC8848127.
