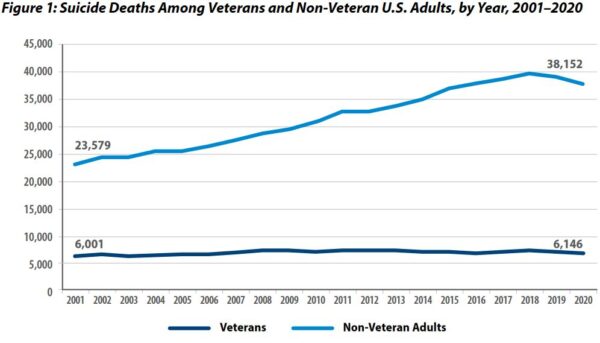
Click to Enlarge: Source: Department of Veterans Affairs (VA) 2022 National Veteran Suicide Prevention Annual Report
BOSTON — VHA facilities appear to have limited staff who can provide mental health care services, and increasing mental health staffing could reduce suicide-related events in veterans, according to a new study.
The study published in the journal Health Services Research aimed to determine the effects of changes in VHA mental health services staffing levels on suicide-related events among a cohort of veterans.1
In 2018, suicide was the 10th-leading cause of death in the United States and the second-leading cause of death for people between 10 and 34 years old. Suicide rates have been increasing for two decades, along with a national shortage of mental health professionals. More than 75% of U.S. counties have a mental health provider shortage, with over half of needs unmet. In addition, more than 90% of Federally Qualified Health Centers are estimated to be incapable of meeting patients’ mental health needs, according to the study.
This significant shortage of mental health providers has led to theories that mental health provider staffing may have a direct impact on suicide rates.
In this study, the researchers focused on veterans who recently separated from active duty service (between 2010 and 2017) and used combined data from the VHA’s corporate data warehouse as well as data from the Department of Defense. A total of 109,376 veterans participated in the study.
For the five-year period from July 2014 to June 2018, the study measured whether a veteran experienced a suicide-related event in each two-week pay period. Suicide-related events included suicidal self-directed violence, suicide attempts, suicide and self-directed violence with undetermined intent.
The researchers identified suicide-related events through the VA-Suicide Prevention and Application Network, the VA Comprehensive Suicide Risk Evaluation and the Suicide Behavior and Overdose Report. These data are collected by the VHA’s Program Evaluation and Resource Center and the Office of Mental Health and Suicide Prevention and are based on notes in a patient’s record from clinicians and suicide prevention coordinators.
The majority of the veterans in the study came from the Army branch (66%), had four or more mental health visits during their service (73%) and had at least one dependent (73%).
The study examined mental health provider staffing per 10,000 enrollees.
“Our findings suggest that increasing mental health staffing at certain facilities in the VHA could help reduce suicide-related events among veterans,” lead author Yevgeniy Feyman, a PhD candidate at the Boston University School of Public Health and a graduate fellow at the Partnered Evidence Based Resource Center at the Boston VA Healthcare System, told U.S. Medicine. “This effect was strongest among facilities that had relatively less staff compared to the number of veterans they serve.”
“We found that, on average, a 1% increase in staffing leads to a 1.6% reduction in suicide-related events. In facilities that were relatively understaffed, we estimated that this would lead to over a 2% reduction. These are very large effect sizes that suggest a high return on investment for mental health staffing.”
The VHA provides an important setting for examining the relationship between mental health provider staffing and outcomes, because the healthcare system has a substantial number of mental health providers already. More than 14% of clinical providers are psychiatrists or psychologists. Also, veterans tend to be disproportionately represented among suicides in the U.S.
Feyman noted that the VHA has put a lot of effort into increasing mental health staffing over the past decade and is better staffed than many other health systems. However, there also has been an increase in veteran suicides.
“Our results underscore the fact that, even in a well-staffed health system, increasing mental health staffing can pay off,” Feyman wrote in an email. “We also contribute new measurement methods to better understand how well-staffed a particular facility or health system really is.”
Increasing mental health staffing is challenging, because the VHA has a fixed annual budget. Individual facilities are responsible for bringing on staffing at the local level, and then facilities are limited by the existing pool of practitioners. The study suggests, however, that some reallocation of existing staff to understaffed facilities might be beneficial, Feyman explained.
“For the VHA, increasing staffing in targeted ways would be incredibly helpful,” Feyman noted. “But we think there are implications for other health systems, too. All major health systems and academic medical centers are interested in better allocating resources. Our approach to measuring staff allocation and the extent of understaffing can be applied by any large health system with similar data to the VHA. However, the catch is that, for mental health, there’s a limit to the number of available professionals out there. This means that we need to do a better job of training mental health professionals and compensating them fairly.”
Understanding the direct impact of changes in mental health provider staffing in the VHA will be critical as policy-makers and health practitioners aim to set optimal staffing levels and ultimately reduce the incidence of suicide in patient populations more generally, according to the study.
The study had several limitations. Because of the high prevalence of mental health conditions among the veteran population, the results might not generalize to other health systems or populations. Also, the sample is limited to a cohort of veterans who were separated from service between 2014 and 2018. Although the sample is diverse among many socio-demographics, caution should be taken in generalizing the findings to veterans who were separated from service outside the study period. In addition, veterans often use non-VHA health services, and these data aren’t included in the analysis.
- Feyman Y, Figueroa SM, Yuan Y, Price ME, Kabdiyeva A, Nebeker JR, Ward MC, Shafer PR, Pizer SD, Strombotne KL. Effect of mental health staffing inputs on suicide-related events. Health Serv Res. 2022 Sep 11. doi: 10.1111/1475-6773.14064. Epub ahead of print. PMID: 36089760.
