Use Increased Even in Patients Without Previous Alcohol Issues
DURHAM, NC — Concerns about long-term effects after bariatric surgery have been heightened by a new study suggesting that unhealthy alcohol use in veterans was much more common after undergoing a bariatric surgical procedure.
What made the findings especially concerning is that those patients did not have unhealthy alcohol use at baseline and were compared with similar ones who did not have weight-loss surgery, according to the article in JAMA Network Open.1
The cohort study of 2,608 VA patients who underwent a bariatric surgical procedure determined that the mean alcohol screening scores in patients without baseline unhealthy alcohol use and the probability of unhealthy alcohol use both increased significantly three to eight years after the procedure. At the same time, reported researchers from the Durham, NC, VAMC, and Duke University, the probability of no alcohol use decreased significantly five to eight years after the procedure.
“From these findings, we estimate that for every 21 patients who undergo an RYGB and every 29 patients who undergo an LSG, on average one from each group will develop unhealthy alcohol use,” the authors advised.
They also pointed out that, in a small sample of patients with unhealthy alcohol use at baseline, the prevalence of postoperative unhealthy alcohol use was higher for patients undergoing gastric bypass than controls.
“Findings of this study suggest that unhealthy alcohol use was much more common after undergoing a bariatric surgical procedure in patients without unhealthy alcohol use at baseline compared with those who did not undergo a procedure,” the authors wrote.
Background information in the article noted that bariatric surgical procedures have been associated with increased risk of unhealthy alcohol use, although no previous research has evaluated the long-term alcohol-related risks after laparoscopic sleeve gastrectomy (LSG), which is currently the most common bariatric procedure. In addition, no United States-based study had compared long-term alcohol-related outcomes between patients who have undergone Roux-en-Y gastric bypass (RYGB) and those who have not.
For the retrospective cohort study, researchers analyzed electronic health record (EHR) data on military veterans who underwent a bariatric surgical procedure at any of the bariatric centers in the VA health system between Oct. 1, 2008, and Sept. 30, 2016. The trial matched surgical patients with nonsurgical control patients with similar alcohol use histories. Data were analyzed in February 2020. Of the surgical patients, 1,684 underwent LSG, and 924 had RYGB.
The study team estimated mean alcohol use, unhealthy alcohol use, and no alcohol use using scores from the validated 3-item Alcohol Use Disorders Identification Test-Consumption (AUDIT-C), which had been documented in the VA EHR.
The final cohort included 2,608 surgical patients—1,964 male [75.3%] and 644 female [24.7%] veterans. Mean (SD) age of surgical patients was 53.0 (9.9) years and 53.6 (9.9) years for the matched nonsurgical patients.
Results indicated that, in patients without baseline unhealthy alcohol use, the mean AUDIT-C scores and the probability of unhealthy alcohol use both increased significantly three to eight years after an LSG or an RYGB, compared with control patients. Researchers explained how, eight years after an LSG, the probability of unhealthy alcohol use was higher in surgical vs. control patients (7.9% [95% CI, 6.4-9.5] vs. 4.5% [95% CI, 4.1-4.9]; difference, 3.4% [95% CI, 1.8-5.0]). The study also determined that, eight years after an RYGB, the probability of unhealthy alcohol use was higher in surgical vs control patients (9.2% [95% CI, 8.0-10.3] vs. 4.4% [95% CI, 4.1-4.6]; difference, 4.8% [95% CI, 3.6-5.9]).
Health Risks
The report emphasized that, while bariatric surgical procedures are associated with well-documented advantages, including sustained weight loss and remission in macrovascular and microvascular conditions, the procedures also have been linked to health risks. Among those are increased unhealthy alcohol use, which ranges from drinking at levels that increase the risk of health consequences to severe alcohol use disorders, which are associated with extensive disability and death, according to the authors.
“To date, most research on alcohol-related risks after a bariatric surgical procedure has been limited to laboratory studies and uncontrolled cohort studies,” the researchers pointed out, adding that, in addition, most patients in past studies had been women. “Understanding alcohol-related risks associated with bariatric surgical procedures in men, who have higher rates of unhealthy alcohol use and alcohol use disorder, is also important,” they wrote.
That’s why they embarked on the study to compare alcohol-related outcomes between patients who underwent an LSG or an RYGB and nonsurgical control patients specifically at the VA. Another advantage to using that cohort is that, annually since 2004, the VA has required screening of all outpatients using the validated three-item Alcohol Use Disorders Identification Test-Consumption (AUDIT-C), producing electronic health record (EHR) data for monitoring alcohol use and unhealthy alcohol use over time.
“In 91.8% of patients not screening positive for unhealthy alcohol use in the two years before the surgical date, patterns of alcohol use and unhealthy alcohol use were similar after LSG and RYGB: both mean alcohol use and the prevalence of unhealthy alcohol use increased after bariatric surgical procedures,” researchers noted. “Eight years after the procedure, patients who had an LSG without baseline unhealthy alcohol use had a 3.5% higher risk of unhealthy alcohol use than control patients, and those who underwent an RYGB had a 4.8% higher risk of unhealthy alcohol use than control patients.”
With alcohol-related risks somewhat more pronounced after RYGB than LSG, the authors suggested that potentially reflected greater changes in alcohol pharmacokinetics.
Researchers recommended that, because of the clinical implications of their results patients undergoing bariatric surgical procedures should be cautioned that drinking alcohol can escalate after bariatric surgery, even in patients with no previous evidence of drinking alcohol above recommended limits.
“Although no expert consensus exists on the recommended limits for those who drink alcohol, not drinking alcohol is the safest option after a bariatric surgical procedure, given that blood alcohol concentration (and therefore the brain’s alcohol exposure) peaks at higher levels after a bariatric operation,” they advised. “Furthermore, all patients who undergo bariatric surgical procedures should be monitored long-term for unhealthy alcohol use, which can be detected with the 3-item AUDIT-C scale.”
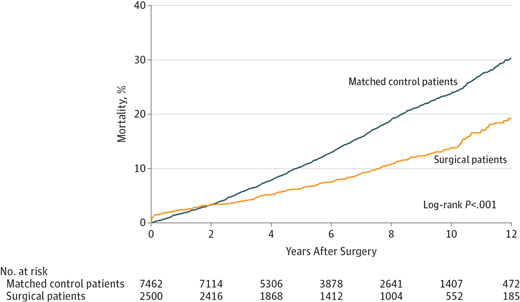
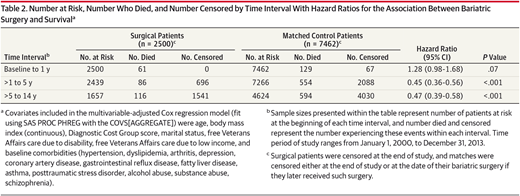
The VA is committed to offering bariatric surgery, partly based on a 2015 study by agency researchers finding that the procedure helps severely overweight patients live longer.2
That study, which involved 10,000 VA patients throughout the nation, found that the 2,500 veterans who had the surgery had a 53% lower risk of dying from any cause five to 10 years after the procedure, compared with 7,500 other severely overweight veterans who had not undergone the procedure.
That was the case, even though patients involved in the research were older, with a mean age of 52, and were 74% male; most, 55%, also had diabetes and many other chronic conditions.
A VA study two years ago did not find, however, that the surgery lowered healthcare costs. The cohort study of 9,954 veterans with severe obesity, total health care expenditures were higher in the three years before surgery and the first two years after surgery among patients who underwent surgery compared with those who did not. Researchers documented that expenditures of patients who did and did not undergo bariatric surgery converged five to 10 years after surgery, explaining, “The value of bariatric surgery lies primarily in its association with improvements in health and not in its potential to decrease health care costs.”3
- Maciejewski ML, Smith VA, Berkowitz TSZ, Arterburn DE, Mitchell JE, Olsen MK, Liu CF, Livingston EH, Funk LM, Adeyemo A, Bradley KA. Association of Bariatric Surgical Procedures With Changes in Unhealthy Alcohol Use Among US Veterans. JAMA Netw Open. 2020 Dec 1;3(12):e2028117. doi: 10.1001/jamanetworkopen.2020.28117. PMID: 33346846; PMCID: PMC7753905.
- Arterburn DE, Olsen MK, Smith VA, Livingston EH, Van Scoyoc L, Yancy WS Jr, Eid G, Weidenbacher H, Maciejewski ML. Association between bariatric surgery and long-term survival. JAMA. 2015 Jan 6;313(1):62-70. doi: 10.1001/jama.2014.16968. PMID: 25562267.
- Smith VA, Arterburn DE, Berkowitz TSZ, Olsen MK, Livingston EH, Yancy WS Jr, Weidenbacher HJ, Maciejewski ML. Association Between Bariatric Surgery and Long-term Health Care Expenditures Among Veterans With Severe Obesity. JAMA Surg. 2019 Dec 1;154(12):e193732. doi: 10.1001/jamasurg.2019.3732. Epub 2019 Dec 18. PMID: 31664427; PMCID: PMC6822094.