Study Calls for VA Intervention to Lower Rates
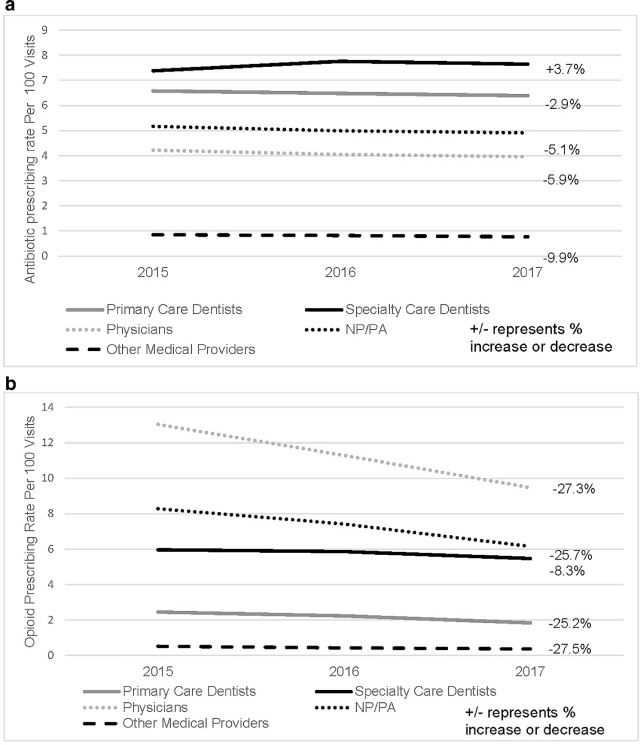
Click to Enlarge: Outpatient Prescribing of Antibiotics and Opioids by Veterans Health Administration Providers, 2015–2017.
Medical and dental providers who are high prescribers of antibiotics are also likely to be high prescribers of opioids, according to a new study.
The national cross-sectional study in Pharmacotherapy assessed the association between high antibiotic and high opioid prescribing by provider type. The study used 2015-2017 electronic health record data from the VA’s Corporate Data Warehouse, a national repository of healthcare encounter data across 170 VA medical centers and 1,074 outpatient facilities.1
The providers in the study were 1,346 dentists and medical providers, including 23,072 physicians, 7,705 advanced practice providers and 3,674 other providers, such as pharmacists and chiropractors.
“Our results indicate that high prescribers of antibiotics are also likely to be high prescribers of opioids,” study author Katie J. Suda, PharmD, MS, research health scientist and associate director of clinical therapeutics in the Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System, told U.S. Medicine. “For dentists, high prescribers of antibiotics had over eight times the odds of being a high prescriber of opioids. For medical providers, high prescribers of antibiotics had nearly three times the odds of being a high prescriber of opioids.”
Nearly 1 in 10 of all providers were high prescribers of both antibiotics and opioids, with 1 in 6 specialty-care dentists being high prescribers of both medications, the study reported. Medical providers prescribed 4,348,670 antibiotic and 10,256,706 opioid prescriptions. Dentists prescribed 277,170 antibiotic and 124,103 opioid prescriptions.
Possible reasons for the link in prescribing of these two medication classes are the conditions treated by the prescriber, the complexity of the patients (sicker patients), past training, adherence to guidelines or prescribing behavior, Suda explained in an email.
“However, we may be able to decrease the use of both medication classes by targeting interventions that focus on antibiotics and opioids,” wrote Suda, who also is a professor of medicine, pharmacy & therapeutics and clinical & translational sciences at the University of Pittsburgh School of Medicine. “Targeting both medication classes could be a key strategy for reducing high prescribing of antibiotics and opioids for both dentists and medical providers. Our results suggest that high prescribing is not due to an overarching facility-level culture of prescribing, and indicates that unique interventions targeted to each type of provider group is needed.”
“High” prescribing versus “low” prescribing for opioids and antibiotics was based on previous research using percentile rankings. High prescribing was defined as being in the top 25% for the visit-based rate of prescriptions for antibiotics or opioids by each provider type and year of prescription. The study notes the rate for being in the top 25% of prescribing for opioids is different for primary care dentists compared to specialty dentists.
The visit-based rate for prescribing was calculated as the number of prescriptions for antibiotics or opioids divided by the number of dental or medical outpatient visits. Providers who had a rate of prescribing in the top 25% for their provider type category were considered high prescribers.
Characteristics of High Prescribers
The analyses identified characteristics of providers who were high prescribers. In medical providers, older provider age, U.S. geographic region, lower VA facility complexity and rural VA facility location were associated with high opioid prescribing. In dentists, factors associated with high prescribing of opioids were younger provider age, male gender, U.S. geographic region and lower number of dentists in a facility, Suda explained.
“Interestingly, at the facility level, dental providers who were high prescribers of antibiotics or opioids were not at the same VA facilities as medical providers who were high prescribers of antibiotics or opioids, respectively,” Suda advised.
Primary care dentists who were high prescribers were also at different facilities from specialty care dentists who were high prescribers (antibiotics p < 0.002, opioids p < 0.0004). In addition, high prescribing physicians were at different facilities than other high prescribing medical providers (advanced practice providers) for both antibiotic and opioid prescribing (p < 0.0001 for both).
This study is significant because there are no other national datasets available to compare prescribing by dentists and medical providers. This is the first study to assess if high opioid prescribing is linked to high antibiotic prescribing and provides comparisons across provider groups.
The study has several key findings. First, there might be an opportunity to improve evidence-based prescribing by targeting multiple drug classes. Secondly, when targeting interventions at the facility-level, prescribing rates by provider type should be assessed so provider groups aren’t left out (i.e., focusing only on physician prescribing and not including dentists). Lastly, dentists are an important component of health systems. Because dentists primarily treat and prevent pain and infection (such as cavities), dentists mainly prescribe antibiotics and analgesics. Dentists need to be provided customized resources to guide prescribing of antibiotics and opioids for oral conditions, Suda explained.
The study did not determine whether providers who met the definition of “high prescribing” were prescribing according to guidelines. However, there is data from the VA and the private sector that these medications are sometimes unnecessarily prescribed. Many national initiatives are focused on decreasing the prescribing of antibiotics and opioids due to serious adverse events associated with their use. In the VA, these initiatives include the Antimicrobial Stewardship Task Force and the Opioid Safety Initiative.
Several initiatives have been implemented over the last few years by the VA to reduce opioid prescribing, including 2019 guidelines for the management of acute pain after dental procedures. These guidelines were the first national guidelines on the treatment of acute oral pain.
“Antimicrobial stewardship initiatives have also been implemented in the VA in medical providers,” Suda added. “We are working now to customize antibiotic stewardship resources to dentists.”
- Evans CT, Fitzpatrick MA, Poggensee L, Gonzalez B, Gibson G, Jurasic MM, Echevarria K, McGregor JC, Gellad WF, Suda KJ. High prescribing of antibiotics is associated with high prescribing of opioids in medical and dental providers. Pharmacotherapy. 2022 Sep;42(9):716-723. doi: 10.1002/phar.2720. Epub 2022 Aug 8. PMID: 35869691.
