Click to Enlarge: Association Between Modality and 90-Day Retention Among VHA Patients Who Received Buprenorphine Following COVID-19–Related Changes Source: Jama Network Open
ANN ARBOR, MI — When the COVID-19 pandemic prompted federal policy changes increasing the use of telehealth delivery, one of those was the increased delivery of buprenorphine—a first-line treatment for opioid-use disorder (OUD) that is known to prevent overdose death and can be prescribed in office-based settings.
These changes included eliminating the required initial in-person visit before a patient could be transitioned to telehealth under the public health emergency exception of the Ryan Haight Online Pharmacy Consumer Protection Act. Additionally, updated guidance from the Drug Enforcement Administration (DEA) and Substance Abuse and Mental Health Services Administration (SAMHSA) allowed—for the first time—buprenorphine visits for new and existing patients to be delivered by telephone (i.e., audio-only).
Today, as policymakers and healthcare leaders debate whether to maintain or roll back policies that have increased flexibility in buprenorphine delivery, many providers, including addiction psychiatrist Allison Lin, MD, MS, are concerned that doing so would leave vulnerable populations—including many veterans—at risk of stopping this potentially lifesaving treatment.
“Helping veterans with opioid-use disorder stay in care is a huge challenge, and I have seen this firsthand with my patients,” said Lin, a research scientist and staff physician at the Center for Clinical Management Research, VA Ann Arbor Healthcare System and senior author of a new study examining the use of telemedicine for the treatment of OUD during the pandemic. “Many folks do not have access to reliable transportation and also have a lot going on in their lives. At the same time, it is critical for people to stay on the medication, buprenorphine. It only helps when patients are taking it. Risk for relapse and overdose often increases substantially when patients stop.”
To inform decisions concerning the continued use or rollback of telemedicine, it is important to understand the potential relationship of buprenorphine treatment modality (video, telephone or in-person) with treatment outcomes, as well as the characteristics of patients who are more or less likely to access different modalities, Lin and her colleagues wrote in JAMA Network Open.1
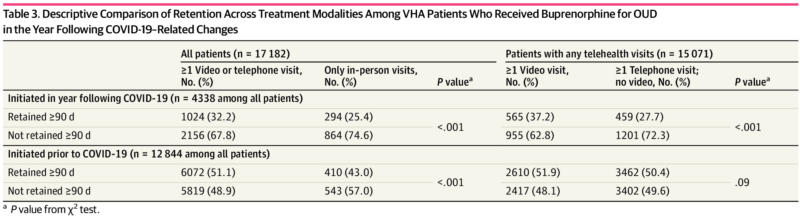
The researchers sought to gain that understanding by examining healthcare data from veterans with OUD receiving buprenorphine treatment in the VHA from March 23, 2020, to March 22, 2021—the year after the start of the pandemic. They then compared the characteristics of patients, including how long they stayed on the medication buprenorphine across three groups: patients who received any video visits for buprenorphine treatment, patients who received telephone but no video visits and patients who only received in-person visits.
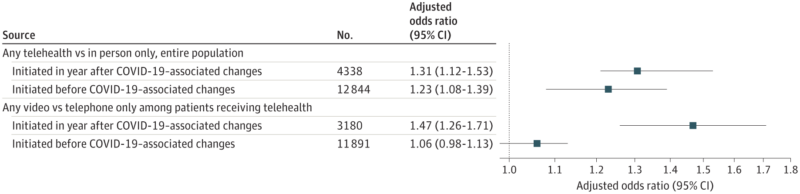
“We found that receiving telehealth-delivered buprenorphine care in the study period was associated with higher likelihood of veterans staying on their treatment at least 90 days or longer,” Lin told U.S. Medicine. “At the same time, there were some differences in who received telehealth or not and who received video versus only phone visits.”
Who Receives Telehealth?
Specifically, patients who were younger, Black, unknown race, Hispanic, nonservice connected or had specific mental health/substance use comorbidities were less likely to receive any telehealth, the study found. Among patients who received telehealth, those who were older, male, Black, nonservice-connected or experiencing homelessness and/or housing instability were less likely to have video visits. Retention was significantly higher for patients with telehealth compared with only in-person visits, regardless of initiation time. Among patients with telehealth, higher retention was observed in those with video visits compared with only telephone for patients who initiated in the year following COVID-19.
“Although, from experiences in clinic, we thought telehealth might help some people stay on their buprenorphine treatment longer, it was still surprising to find that was true on average,” said Lin. “Also, we know that the VHA has probably invested more than any other healthcare system in the country to help people access telehealth—for example by providing technical support and tablets to help veterans connect—yet, it was interesting to see that there were still differences in which veterans used telehealth to access care.”
For many veterans struggling with OUD, buprenorphine is one of the only treatments that has been found to help reduce risk for overdose and regain their lives, yet the majority of veterans are not receiving this treatment and struggle to stay on the treatment long term, Lin said. “As a country, we are working hard on trying to find ways to help more people get this treatment and telehealth seems like a potentially important option, and the VHA is at the forefront of advancing access to telehealth, so this tool can be potentially even more promising for veterans.”
Lin said she hopes the findings of this and other studies will provide concrete data to guide some of the policy discussions concerning the continued availability of buprenorphine by telehealth, noting that the discontinuation of telehealth would disproportionately affect certain groups of patients—especially those who are older, Black and experiencing homelessness and/or housing instability.
“Telehealth was not an option for many patients pre-pandemic,” Lin explained. “What I hope, moving forward, is that veterans and clinicians have more choices, including telehealth, and research can, hopefully, help us understand veteran and clinician experiences and preferences and tell us more about which patients may benefit from telehealth or in-person care.”
- Frost MC, Zhang L, Kim HM, Lin LA. Use of and Retention on Video, Telephone, and In-Person Buprenorphine Treatment for Opioid Use Disorder During the COVID-19 Pandemic. JAMA Netw Open. 2022 Oct 3;5(10):e2236298. doi: 10.1001/jamanetworkopen.2022.36298. PMID: 36223118; PMCID: PMC9557869.