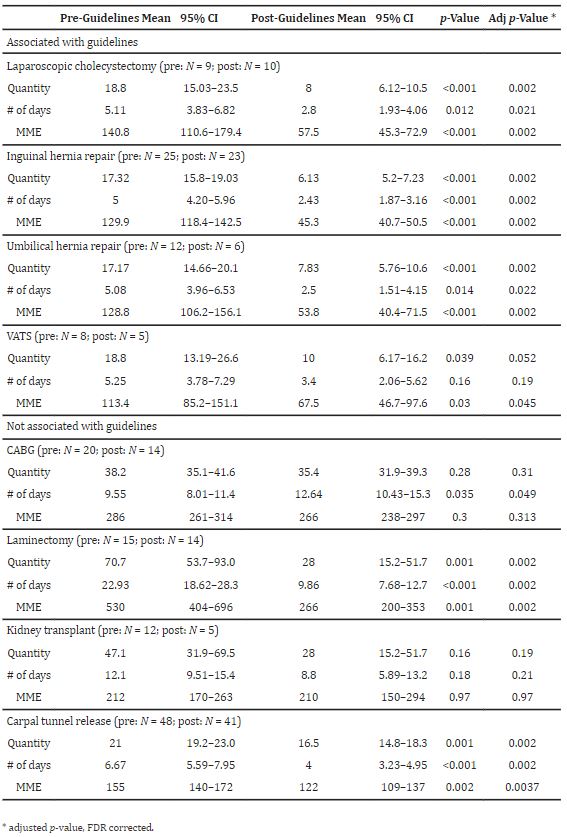
Click to Enlarge: Pre- and post- guideline opioid prescribing in procedures with and without associated guidelines. Source: Journal of Clinical Medicine
PITTSBURGH — Drug overdose is the leading cause of injury-related death in the United States. For many, initial exposure to opioids occurs in the hospital following surgery, and current studies show that up to 75% of post-operative patients have unused opioid pills after discharge. Thus, it’s important that efforts to reduce opioid over-prescription and overdoses begin in the hospital, according to authors of a new study that aims to target the opioid crisis at its inception.
“Although inadequate pain control can lead to decreased mobility and higher readmission rates, research shows this excess indicates that current prescribing patterns overcompensate for pain control,” wrote the authors of the study published in the Journal of Clinical Medicine. “Providers not tailoring opioid prescriptions to procedure or inpatient opioid use may contribute to this overcompensation.”1
In response to this growing dilemma, the VA implemented the Opioid Safety Initiative in 2013, which disseminates best practices for prescribers, patient overdose prevention education and prescription-tracking. This initiative led to decreased opioid prescriptions after total knee arthroplasty.
The new study, led by Rajeev Dhupar, MD, MBA, chief of thoracic surgery at VA Pittsburgh Healthcare System and associate professor at University of Pittsburgh School of Medicine, builds on that earlier effort by aiming to decrease the number of opioids in circulation by guiding clinicians to adopt more thoughtful post-operative prescribing practices through the creation and implementation of multidisciplinary, clinician-tailored and patient-centered post-operative opioid prescription order sets.
“We wanted to ensure that we were prioritizing all aspects of safety for our veterans by following best practices for limiting the over-prescribing of narcotics after surgery,” Dhupar said.
Dhupar and his colleagues began this process by examining prescribing practices in the Pittsburgh Veterans Affairs Health System over a several-month period, he said. Once they identified key areas where they could improve as an institution, they created a task force to develop guidelines for patients undergoing both inpatient and common outpatient procedures. Bundled order sets were created and incorporated into the provider workflow in CPRS—the VA electronic medical system, from these guidelines. In addition to the order set, 30-minute annual education sessions for the prescribers were implemented to demonstrate the order set and discuss the rationale.
The researchers then conducted a retrospective, observational study to investigate the change in in post-operative opioid prescribing after guideline implementation Quantity of opioid pills and number of days of the prescription were collected by the pharmacy department for all procedures over three-month intervals both pre- and post-guideline implementation. The total morphine milligram equivalents (MME) for each prescription were calculated based on quantity of opioid pills and number of days.
Their key finding: “Prescriber education and easy-to-follow orders can reduce excessive opioid prescribing,” Dhupar said.
After implementation of opioid-prescribing guidelines, most procedures with associated post-operative opioid-prescribing guidelines preceded a decrease in opioid prescribing. MMEs, quantity of pills prescribed and days prescribed were statistically significantly reduced for cholecystectomy, inguinal hernia repair and umbilical hernia repair. Most procedures without associated post-operative opioid prescribing guidelines—Coronary artery bypass grafting (CABG), laminectomy and carpal tunnel release—also preceded changes in opioid prescribing, the study found.
“This study documents the first post-operative opioid prescribing guidelines in a Veteran surgical population,” the authors wrote. “When informally queried, providers who used the guidelines reported that they aided in provider workflow and made prescribing a more efficient process. Additional benefit was seen with intern and resident physicians who did not have experience with opioid prescribing. Ultimately, guidelines assisted naïve providers in prescribing appropriate number and days of opioids.”
“We felt that this program would be successful, because most providers want to reduce unnecessary dispensing of opioids and the order sets and education were successful at facilitating this,” said Dhupar. “The findings demonstrate we can provide better care with thoughtful collaborative efforts that include education.”
- Hlavin C, Muluk S, Muluk V, Ryan J, Wagner J, Dhupar R. A Program to Reduce Post-Operative Opioid Prescribing at a Veterans Affairs Hospital. J Clin Med. 2022 Sep 16;11(18):5453. doi: 10.3390/jcm11185453. PMID: 36143098; PMCID: PMC9506192.
