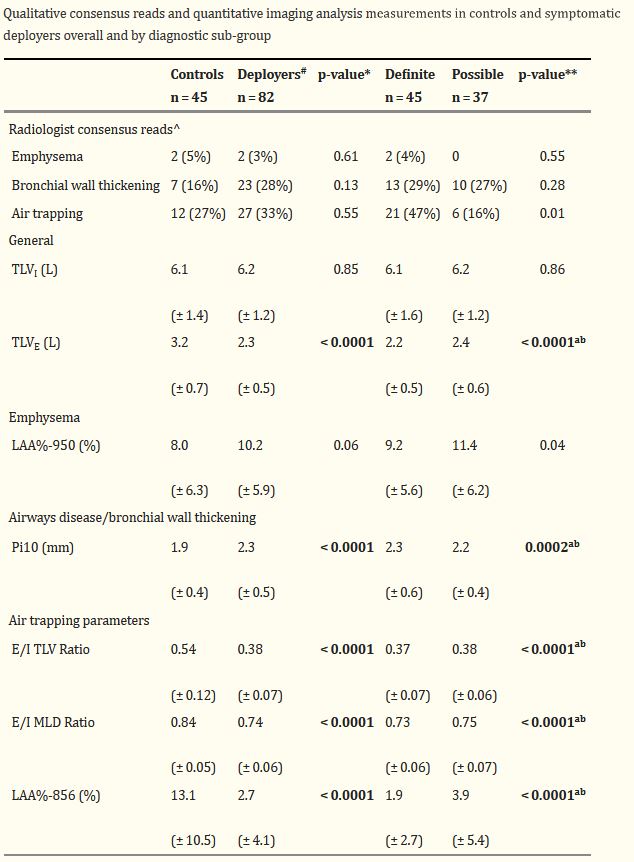
Click To Enlarge: Bold values are statistically significant
Results are the count (percentage) or mean (± standard deviation)
^ Radiologist consensus reads were not available for two controls and two deployers that were included in the analysis after original review by the radiology team
# Expiratory quantitative imaging values were not able to be calculated for 20 deployers
* Deployers and controls were compared using t-tests (Satterthwaite result) for continuous variables and Fisher’s exact tests for categorical variables. Statistically significant p-values are bolded if < 0.005, adjusting for multiple comparisons (10 tests) with a Bonferroni correction
** Diagnostic groups were compared using ANOVA for continuous variables and Fisher’s exact tests for categorical variables. Statistically significant p-values are bolded if < 0.005, adjusting for multiple comparisons (10 tests) with a Bonferroni correction. Individual comparisons between groups were performed if the overall test was significant after Bonferroni correction with the following designations for significant differences (p < 0.05): a definite vs controls, b possible vs controls, c definite vs possible Source: National Library of Medicine
DENVER — Quantitative imaging analysis has been able to detect airway abnormalities in military personnel with persistent respiratory symptoms, offering a new, effective tool to diagnose and monitor patients with deployment-related lung disease, according to a recent study.
Military personnel who have inhaled hazardous particulate matter from burn pit emissions, desert dust, occupational vapors, dusts, gases and fumes (VDGF), explosive blasts and diesel exhaust during deployment to Iraq, Afghanistan and other Southwest Asia locations may be at increased risk for respiratory diseases. Deployment-related asthma, bronchiolitis and persistent, occasionally career-ending, respiratory symptoms have been reported in military personnel deployed to these environments since Sept. 11, 2001.
These military personnel sometimes face challenges when they seek care, because their pulmonary function tests and qualitative visual assessment of high resolution computed tomography (HRCT) findings are often normal or nonspecific, however. Therefore, more sensitive diagnostic markers of lung disease are needed.
This study, published in the journal BMC Pulmonary Medicine, explored the use of quantitative HRCT imaging markers of large and small airways abnormalities, including airway wall thickness, emphysema and air trapping, in previously deployed military personnel with clinically-confirmed lung disease.i
In addition to healthy controls, study participants included previously deployed military personnel who were seen as patients in the Center for Deployment-Related Lung Disease at National Jewish Health in Denver and were evaluated for persistent respiratory symptoms that began during or after post-9/11 deployment to Southwest Asia. Medical and occupational histories were collected along with their chest CT images for quantitative analysis.
Chest HRCT images from 45 healthy controls and 82 symptomatic, previously deployed military personnel with asthma, distal lung disease or both were analyzed to calculate airway wall thickness (by Pi10), emphysema (by percentage of lung volume with attenuation < -950 Hounsfield units [LAA%-950]), and three parameters of air trapping (expiratory/inspiratory total lung volume and mean lung density ratios, and LAA%-856).
“Our study used several quantitative parameters on high resolution chest computed tomography (CT) images that measure the thickness of the small airways, emphysema and air trapping,” Cecil S. Rose, MD, senior author of the study, a physician at National Jewish Health in Denver and a professor at the University of Colorado, told U.S. Medicine. “While spirometry can detect lung injury that is more advanced, subtle changes are difficult to detect without more sensitive tools such as quantitative chest imaging.”
Appearing Healthy
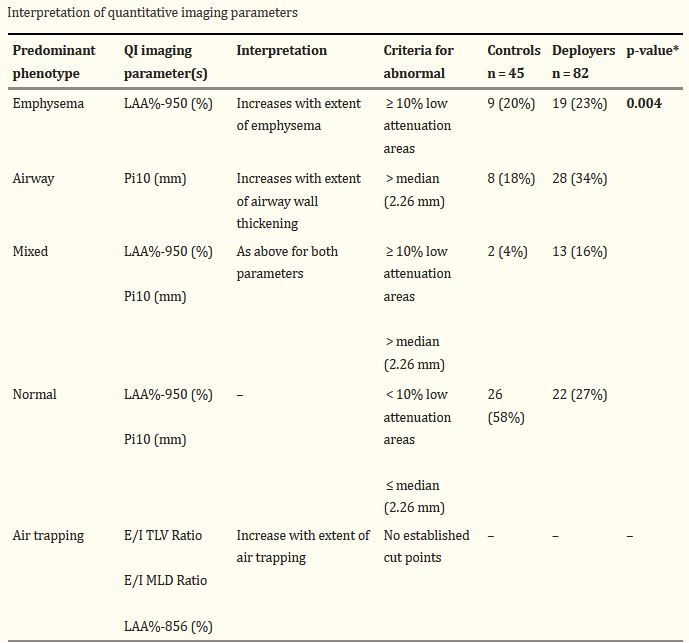
Click To Enlarge: Bold value is statistically significant
Results are the number (%)
* Deployers and controls were compared using Chi square tests Source: National Library of Medicine
Spirometry, the most commonly used lung function test that measures the size of a person’s lungs at full inspiration and how well they can forcibly exhale air, appears insensitive for military personnel with respiratory problems. In some of these patients, spirometry can’t reliably measure the very small airways (bronchioles). In addition, military personnel are typically physically fit at baseline, so changes in lung function following military deployment may not decline below the lower limit of normal. Consequently, those with post-deployment respiratory symptoms may still appear healthy and “within normal limits” on spirometry testing, Rose explained in an email.
The study found that spirometric measures were not statistically significantly different between the healthy controls and symptomatic, previously deployed military personnel. Quantitative chest HRCT imaging analysis identified emphysema in deployees with asthma and distal lung disease, and this method may be useful in detecting and monitoring deployment-related lung disease in a population where spirometry is typically normal.
“Our study results are significant because they provide evidence showing that quantitative chest CT image analysis may aid in diagnosis and monitoring of patients with deployment-related lung disease,” Rose wrote. “Quantitative image analysis of chest CT scans may be helpful to show subtle findings of airway injury, including bronchial wall thickening, emphysema and air trapping in previously deployed military personnel.”
While the study had several limitations, it is the first to demonstrate the potential value of quantitative analysis of HRCT in a population of symptomatic military deployees with large and small airways disease. The findings have important implications for the diagnosis and management of respiratory diseases.
“While quantitative imaging analysis is not widely available clinically, it may be in the future and may improve diagnosis of distal lung and small airways abnormalities in many different respiratory diseases,” Rose explained. “It is important to identify reliable noninvasive tools to aid in clinical diagnosis and management of military personnel with respiratory symptoms following deployment.”
Although gender and smoking status were not statistically significantly different between groups, limitations of this study include demographic differences between deployees and controls. Controls were significantly older and had more smoking pack-years, and deployees had higher body mass indexes (BMIs), which may have limited the ability to detect imaging differences between groups. Also, imaging techniques can vary between sites and could have resulted in some measurement error, though this possibility was reduced by consistent training of staff. In addition, quantitative imaging analysis using these techniques is not widely available and requires substantial technical knowledge and expertise.
- Zell-Baran LM, Humphries SM, Moore CM, Lynch DA, Charbonnier JP, Oh AS, Rose CS. Quantitative imaging analysis detects subtle airway abnormalities in symptomatic military deployers. BMC Pulm Med. 2022 Apr 27;22(1):163. doi: 10.1186/s12890-022-01960-w. PMID: 35477425; PMCID: PMC9047334.

