BETHESDA, MD — MHS provides universal healthcare to beneficiaries, reducing barriers to medical care access. That appears to be especially beneficial for military beneficiaries facing a colon cancer diagnosis and treatment.
A new study led by researchers at John P. Murtha Cancer Center Research Program found that access to military medical care leads to longer survival rates compared to those of their counterparts in the general population.1
The study analyzed data from 11,907 patients in the DoD’s Automated Central Tumor Registry (ACTUR) and 23,814 from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program. Each ACTUR patient was matched with two SEER patients with similar—or same—age, race, gender and diagnosis year to minimize the influence of demographic differences on survival. In addition to survival, the researchers compared the two populations in cancer stage at diagnosis, which is one of predictor for cancer survival, said Craig D. Shriver, MD, professor and director of the Murtha Cancer Center Research Program, Department of Surgery, Uniformed Services University of the Health Sciences.
Researchers determined that ACTUR patients were more likely than SEER patients to be diagnosed at an earlier tumor stage (Stage 1) (22.67% vs. 18.64%). ACTUR patients were also less likely than the patients in the SEER database to be diagnosed at a later tumor stage (Stage 4) (18.74% vs. 21.63%).
Overall, the patients with colon cancer in the MHS—which serves uniformed service members, military retirees and family members—had an 18% lower risk of death compared with patients in the general population. This finding was generally consistent across the subgroups defined by age, gender and race.
The researchers noted that the survival benefit tended to be greater for Black patients than that for whites. “Black patients in the MHS were 26% less likely to die than those in the general population, while the corresponding percentage was 18 for white patients,” Shriver pointed out. “This finding suggests the possibility that a universal health care system may be helpful for reducing racial disparity in colon cancer survival.”
Shriver said the greater survival rates among MHS patients were not surprising, considering findings of the group’s earlier research comparing outcomes of ACTUR and SEERS patients on other three other forms of cancer.
- Lung cancer. In a 2018 study of non-small cell lung cancer, ACTUR patients had significant survival advantage that was present regardless of cancer stage, grade, age group, sex or race.
- Glioma. In a 2020 study, which included 2231 glioma cases from ACTUR and 4462 cases from SEER, ACTUR cases exhibited significantly better overall survival than SEER cases. The survival advantage of the ACTUR patients was observed in most subgroups stratified by age, sex, race, diagnosis year and histology. For glioblastoma, the survival advantage was observed in both the pre- and post-temozolomide periods.
- Sarcoma. A study of young sarcoma patients published earlier this year, showed soft tissue sarcoma patients in ACTUR had significantly better overall survival compared with SEER patients, but no significant difference in overall or five-year overall survival between ACTUR and SEER patients with bone sarcoma.
Those study results were what prompted the researchers to determine if the results held true for colon cancer, one of the more common and lethal cancers, he said. “The consistent findings across these studies suggests the benefits of universal healthcare access provided by MHS for improving survival may not be cancer-site specific. Specific factors related to the benefits warrant further research.” Shriver said.
Research on colon cancer is important because colorectal cancer has the third-highest death rate out of all cancers in the United States and is as common in the MHS as in the U.S. population as a whole, he said, adding, “Therefore, it is highly important to improve survival of patients with colon cancer. We hope that our study can help address the significance of universal healthcare for better outcomes of the disease.”
Shriver was part of a study team publishing a study in PLoS One recently discussed incidence of digestive cancers in the military population, especially since the cancers are more common among men and are increasing in adults younger than 50.
“Military population, which is dominantly male and young, and general populations differ in exposure to risk factors for these cancers. However, no studies have systematically investigated whether the incidence rates of these cancers differ between the two populations,” the authors wrote, stating that they sought to compare incidence rates and trends of select digestive cancers between active-duty military and general populations in men aged 20-59 years.
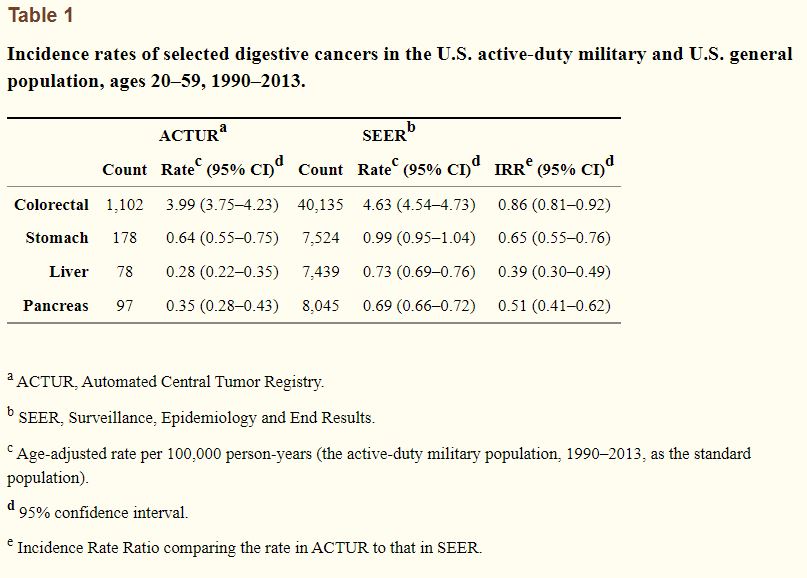
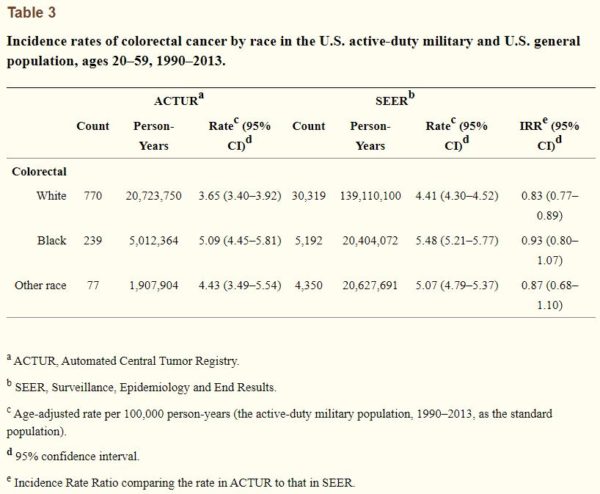
Using ACTUR and SEER data, they compared age-adjusted incidence rates of colorectal, stomach, liver, and pancreatic cancers among men aged 20-59 years between the two populations.
Results indicated that the age-adjusted incidence rates of colorectal, stomach, liver, and pancreatic cancers were overall lower among active-duty servicemembers than SEER patients (IRR = 0.86, 95% CI = 0.81-0.92; IRR = 0.65, 95% CI = 0.55-0.76; IRR = 0.39, 95% CI = 0.30-0.49; IRR = 0.51, 95% CI = 0.41-0.62, respectively).
“This was observed in the groups of both ages 20-39 and 40-59 years for stomach cancer, and in the group of ages 40-59 years for colorectal cancer. The incidence rates of colorectal cancer tended to decrease since 2008 in ACTUR,” they wrote.
The study concluded that incidence rates for selected digestive cancers overall were lower in the active-duty military population than the U.S. general population but added, “This study highlights the need for more research enhancing our understanding of variations in these cancers between the two populations.”
- Lin J, McGlynn KA, Shriver CD, Zhu K. Comparison of Survival among Colon Cancer Patients in the U.S. Military Health System and Patients in the Surveillance, Epidemiology, and End Results (SEER) Program. Cancer Epidemiol Biomarkers Prev. 2021 Jul;30(7):1359-1365. doi: 10.1158/1055-9965.EPI-20-1267
- Bytnar JA, Shriver CD, Zhu K. Incidence rates of digestive cancers among U.S. military servicemen: Comparison with the rates in the general U.S. population. PLoS One. 2021 Sep 3;16(9):e0257087. doi: 10.1371/journal.pone.0257087. PMID: 34478468; PMCID: PMC8415586.