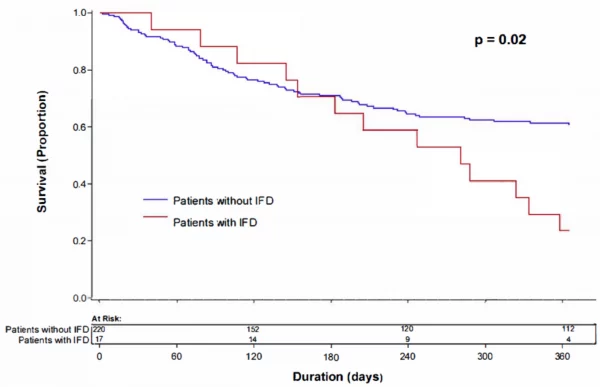
Click To Enlarge: Kaplan-Meier analysis showing survival at one year after the date of first induction therapy for acute myeloid leukemia comparing patients who did or did not have invasive fungal disease.
ANN ARBOR, MI — Invasive fungal disease (IFD) is a highly morbid complication in patients with hematologic conditions including acute myeloid leukemia (AML), whose risk is increased due to both the disease itself and the treatments for it. While studies have demonstrated a benefit of antifungal agents for IFD prophylaxis in patients at high risk, breakthrough cases have been reported in up to 18% of AML patients.
Such reports are concerning, said Kathleen Linder, MD, a clinical assistant professor and infectious disease specialist at the University of Michigan Infectious Disease Clinic who also practices at the Ann Arbor VAMC.
“Our research group has looked into patients with AML in previous studies. However, since we looked in the past, recommendations on prophylaxis regimens to prevent fungal infections have changed,” said Linder, who led a new study on IFD in patients with newly diagnosed AML.1
Changes have been prompted by the recent development of new antifungals and improved formulations of existing agents, Linder and her colleagues wrote in the Journal of Fungi. Additionally, revised definitions for IFD have been developed by the European Organization of Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium (EORTC/MSGERC), and a consensus definition for B-IFD has been published by the MSGERC and the European Confederation of Medical Mycology (ECMM) This new definition for B-IFD incorporates the newer antifungal agents and better defines antifungal exposure by including pharmacokinetic parameters of the prophylactic agents.
“We wanted to see the effect of these changes on our patient population,” she told U.S. Medicine.
Linder and her colleagues identified all (251) adults patients beginning chemotherapy for newly diagnosed AML at the University of Michigan Medical Center from 2014-2019 and followed study patients for one year from the first day of chemotherapy, unless death occurred before that time.
They reviewed:
- Medical records to collect data on patient demographics and comorbidities; AML status at baseline, at time of IFD diagnosis and at the last follow-up;
- Chemotherapy regimens;
- Hematopoietic cell transplantation;
- Graft versus host disease;
- Cumulative duration of neutropenia;
- Cumulative prophylactic antifungal exposure;
- Serum trough concentrations of prophylactic antifungals when available;
- Outcome of IFD and breakthrough IFD at 12 weeks from the date of diagnosis; and
- Overall mortality at one year after first induction chemotherapy.
All received antifungal prophylaxis unless there were contraindications, including intolerance to the agents or involvement in a clinical trials whose protocols prohibited their use. The preferred antifungal prophylaxis for patients undergoing chemotherapy was voriconazole. If intolerance or drug-drug interactions were present, alternative regimens, including posaconazole, isavuconazole, fluconazole or micafungin, were used at the discretion of the hematology team. Acyclovir was given throughout all chemotherapy cycles for antiviral prophylaxis. Bacterial prophylaxis with a fluoroquinolone was given only to patients with relapsed or refractory AML.
More Likely to Die
Of the 251 patients studied, 17, (about 7%)—a percentage lower than that in previous trials—of the patients who started chemo for AML developed a proven or probable fungal infection within the first year, and risk for fungal infection increased with every consecutive day of neutropenia, Linder said. “About half of these patients were not receiving any antifungal prophylaxis when they developed an invasive fungal infection,” she said. “Patients who developed a fungal infection after chemotherapy were more likely to die within that year than those who did not.”
While the goal is zero cases of IFD, Linder said she was surprised that there were not more. “Part of this is probably my bias as an infectious diseases physician; I usually get called once an infection has been identified, so I tend to think of chemotherapy as being more dangerous than it obviously is.” She was also surprised that there were patients who were not on preventive therapy—9 of the 17 (53%) were not. “Several of the infections that were present might have been able to be prevented, if these patients were able to be on prophylaxis against fungal infection.”
Linder said the new study underscores the severity of fungal infections in this population and the value of the new recommendations for prophylaxis.
“The main thing I hope physicians take away from this study is to consider fungal infections in patients after chemotherapy, because they can be difficult to diagnose and lead to high mortality.” She said she also hopes the findings help physicians to consider the value of antifungal prophylaxis in patients beginning treatment for AML.
“Finally,” she said, “since we did see breakthrough infections—although luckily not many—I hope this highlights the need for the development of other antifungal agents that can be used in this setting.”
- Wasylyshyn AI, Linder KA, Kauffman CA, Richards BJ, Maurer SM, Sheffield VM, Colon LB. Invasive Fungal Disease in Patients with Newly Diagnosed Acute Myeloid Leukemia. J. Fungi 2021, 7(9), 761; doi.org/10.3390/jof7090761

