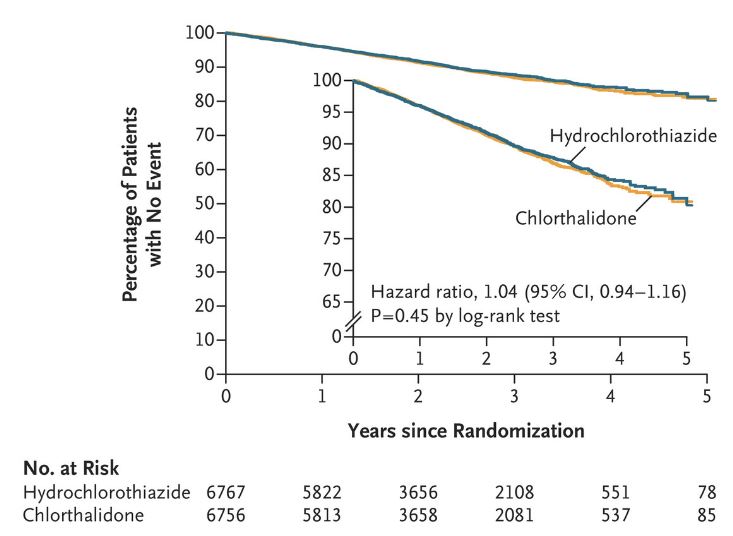
Click to Enlarge: Kaplan–Meier Survival Curve for the Primary Outcome. Source: The New England Journal of Medicine
CHICAGO — In “surprising” results, two common diuretics used to control blood pressure, chlorthalidone and hydrochlorothiazide, had no differences in outcomes for cardiovascular events, including death, in veteran patients, according to a new study.
The Diuretic Comparison Project, presented at the American Heart Association’s Scientific Session 2022 in Chicago and virtually in November and published in The New England Journal of Medicine, compared how these two commonly prescribed blood pressure-lowering medications prevent cardiovascular events in veterans with hypertension. The project is a pragmatic trial that allowed participants and health care professionals to know which medication was being prescribed and to administer the medication in a real-world setting.1
Nearly half of U.S. adults have high blood pressure, a leading cause of heart disease, according to the American Heart Association’s Heart Disease and Stroke Statistics 2022 Update.2 Thiazide diuretics, such as chlorthalidone and hydrochlorothiazide, have been prescribed for more than 50 years and are considered first-line treatment for high blood pressure.
The researchers wanted to evaluate the safety and efficacy of hydrochlorothiazide and chlorthalidone in improving cardiovascular outcomes among patients with hypertension, because no previous studies have compared them.
The study included 13,523 patients recruited from 72 VAMCs, which involved 537 clinics in all 50 states. Among the patients, 45% of individuals resided in rural areas and about 15% were Black or African American. Because this was the VA population, there were few women (3%) in the study.
Participants were over the age of 65 years old, prescribed 25 or 50 mg of hydrochlorothiazide by the VA, and had a mean baseline systolic blood pressure of 139 mm Hg. Patients were randomized into one of two groups, either hydrochlorothiazide at 25 or 50 mg/day, or an equivalent dose of 12.5 or 25 mg/day of chlorthalidone. The study examined rates of heart attack, stroke, heart failure and non-cancer death after follow-up of 2.4 years.
“In our study of about 13,500 individuals, we found no difference in blood pressure over time. We also found no difference in our primary outcome of cardiovascular events or non-cancer death. There was a slight increase in the number of people with labs identified as low potassium in the chlorthalidone group,” Areef Ishani, MD, MS, director of the Minneapolis Primary Care and Specialty Care Integrated Care Community (ICC) at the Minneapolis VA, told U.S. Medicine. Ishani also is director of the Minneapolis VA Midwest Health Care Network’s Specialty Care ICC, as well as vice chair and professor in the Department of Medicine at the University of Minnesota.
The incidence of hypokalemia (low potassium) was higher in the chlorthalidone group than in the hydrochlorothiazide group (6.0% vs. 4.4%, P<0.001).
Many specialists believe that chlorthalidone does a better job controlling blood pressure and is more beneficial in reducing the risks of developing heart disease. Guidelines recommend chlorthalidone to treat hypertension, but most providers use hydrochlorothiazide, Ishani wrote in an email.
This study found no cardiovascular benefit for treatment with chlorthalidone. Patients who received chlorthalidone didn’t have a lower occurrence of major cardiovascular outcome events or non-cancer-related deaths than patients who received hydrochlorothiazide.
Surprised by Results
“We were very surprised with the results,” Ishani explained in an email. “We also believed that chlorthalidone was superior to hydrochlorothiazide. This was based on past studies suggesting that chlorthalidone was better, along with the better 24-hour blood pressure control data for chlorthalidone as compared to hydrochlorothiazide. No study has compared them head to head.”
The researchers determined that chlorthalidone and hydrochlorothiazide have similar effects when used to control blood pressure and prevent cardiovascular disease in doses that were used in this study. The most common dose used was 25 mg of hydrochlorothiazide at baseline, which was used in 95% of the population. Prior studies have shown that at least 50 mg of hydrochlorothiazide is required to reduce cardiovascular disease, Ishani wrote in an email.
“If patients have poor blood pressure control on these low doses, providers should feel free to increase the dose of the thiazide diuretic,” Ishani explained. “A simple way to do this would be to convert the 25 mg of hydrochlorothiazide to 25 mg of chlorthalidone, as chlorthalidone is twice as potent as hydrochlorothiazide.”
The study’s results are significant, because many providers have been unsure which thiazide to use for the prevention of cardiovascular disease. There also have been studies suggesting more adverse effects, such as acute kidney injury and new onset chronic kidney disease with chlorthalidone.
“Providers can use either chlorthalidone or hydrochlorothiazide to treat blood pressure,” Ishani explained in an email. “Both these drugs are available in combination pills. Similarly, the vast majority of VA providers use low doses of thiazide diuretics. If patients have poor blood pressure control, increasing the dose of the thiazide is an effective strategy for attaining blood pressure control. Our results suggest that both drugs have similar effects on blood pressure, cardiovascular outcomes as well as adverse events, in doses that were used throughout the VA.”
In addition, a subgroup analysis suggested a difference in the primary outcome by the presence or absence of prior stroke or heart attack. Among the small group of patients who had a history of heart attack or stroke, those taking chlorthalidone had reduced the risks of heart disease and death by an average of 27%. Because this could be a chance finding, the researchers are unclear how to interpret these results. Further studies are needed to understand the findings.
- Ishani A, Cushman WC, Leatherman SM, Lew RA, et. al. Chlorthalidone vs. Hydrochlorothiazide for Hypertension–Cardiovascular Events. 2022/12/14. New England Journal of Medicine. doi: 10.1056/NEJMoa2212270. https://www.nejm.org/doi/full/10.1056/NEJMoa2212270.
- Tsao CW, Aday AW, Almarzooq ZI, Alonso A, et. al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022 Feb 22;145(8):e153-e639. doi: 10.1161/CIR.0000000000001052. Epub 2022 Jan 26. Erratum in: Circulation. 2022 Sep 6;146(10):e141. PMID: 35078371.

