By: Jennifer Marquez
Click to Enlarge: Antiplatelet Therapy, Statin Use, and Statin Adherence Among Patients With Premature Atherosclerotic Cardiovascular Disease (ASCVD)
HOUSTON — Women veterans with early-onset coronary artery disease are significantly less likely than men to receive medications that can prevent stroke, heart attack or peripheral arterial disease progression, according to a new nationwide study.1
While the overall mortality rate for coronary heart disease has declined over the past 20 years, outcomes for younger patients have worsened. Atherosclerotic cardiovascular disease is the leading cause of death worldwide, and early-onset ASCVD represents a prominent and fast-growing challenge for clinicians and the healthcare system.2
Previous studies in the general civilian population have established sex differences in cardiovascular medication prescription. For example, women are less likely to be prescribed aspirin or statins. However, there has been little research focusing on premature ASCVD patients, particularly veterans, who are at higher risk for cardiovascular disease than nonveterans.3,4
After a patient experiences an ASCVD event—which encompasses a diagnosis of ischemic heart disease (IHD), ischemic cerebrovascular disease (ICVD) or peripheral arterial disease (PAD)—secondary prevention guidelines recommend beginning antiplatelet and statin therapy.
In the recent study, published in JAMA Cardiology, researchers from Michael E. DeBakey VAMC, Baylor College of Medicine, and their colleagues compared secondary prevention between male and female patients with premature ASCVD (occurring at age 55 or younger) and extremely premature ASCVD (occurring at age 40 or younger). They reviewed electronic medical records and clinical data from 147,600 patients enrolled in the Veterans With Premature Atherosclerosis (VITAL) registry who had experienced one early-onset ASCVD event and examined how patients were treated after the event.
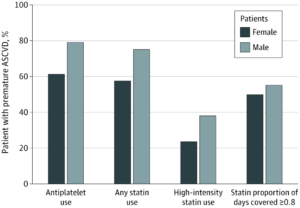
The study found that, compared to men, women received less-aggressive therapy. Women with premature IHD were less likely than men to be prescribed antiplatelet therapy or statins, including high-intensity statins. Among premature IHD patients who were prescribed statins, women had lower medication adherence than men. Similarly, women with premature ICVD and premature PAD also received fewer antiplatelet agents, statins or high-intensity statins than men.
Among patients with extremely premature ASCVD (including those with extremely premature IHD, ICVD and PAD), women received less antiplatelet therapy, statins and high-intensity statins than men. No sex-associated differences in statin adherence among patients with premature ICVD, premature PAD or extremely premature ASCVD were identified, however.
The findings are troubling, given the likelihood of severe outcomes for younger patients, particularly younger female patients, the researchers noted.
“Especially for this young population of patients, subsequent ASCVD events may result in catastrophic morbidity and mortality, drastically reducing their quality of life or lifespan,” said Michelle T. Lee, MD, the study’s first author and an advanced post-doctoral fellow at the Michael E. DeBakey VAMC. “Recent research has also indicated that young women with premature ASCVD suffer from comparatively higher mortality rates than men.”5
Past research has highlighted gender differences in cardiovascular care delivery, including underdiagnosis and subsequent undertreatment in women. The sex-based disparities documented in the new study are potentially magnified by the patients’ relatively young ages, according to Lee, as their disease risk is often under-recognized by providers as well as the patients themselves and their families.6
Among younger patients, psychosocial factors may limit younger patients’ ability to access or navigate the healthcare system. Women of childbearing age may also have increased fears of potential adverse effects from statins.
Additionally, “clinician unawareness and bias plays a large role in what’s known as ‘clinical therapeutic inertia,’ a phenomenon that results in failure to initiate or escalate guideline-concordant care,” Lee said. Indeed, the study found that the youngest patients (those with extremely premature ACSVD) had had the lowest prescription rates. “Yet patients with extremely premature ASCVD stand to gain the most benefit from prevention therapy in potential salvageable ‘Disability Adjusted Life Years,’ improvements in quality-of-life, and costs associated with repeated events,” Lee said.
The researchers noted that, although women were significantly less likely to receive prescriptions, both sexes suffered from drastically low rates of secondary prevention therapy. “Men from the premature and extremely premature cohort also had suboptimal antiplatelet and statin treatment,” explained Lee. “Guideline-recommended high-intensity statin therapy was particularly low among both women and men with premature and extremely premature ASCVD.”
From 2005 to 2015, women enrolled in VA health services nearly doubled to more than 720,000. In the coming years, these numbers are predicted to continue rising, and the researchers say a systems-based approach is necessary to address the sex-based gap in healthcare delivery.7
“Since veteran women face unique social and health risks compared with civilian women, more work is needed to better understand their healthcare needs,” Lee pointed out. “The first step in evaluating drivers of this gender-based care inequality entails qualitative surveys assessing gaps in the healthcare system from viewpoints of patients, prescribers and policymakers. After identifying possible gaps, trials of system-level interventions may be implemented to target and improve guideline-directed therapy practices and medication adherence.”
- Lee MT, Mahtta D, Ramsey DJ, et.al. Sex-Related Disparities in Cardiovascular Health Care Among Patients With Premature Atherosclerotic Cardiovascular Disease. JAMA Cardiology. Published April 21, 2021. doi:10.1001/jamacardio.2021.0683
- Wilmot KA, O’Flaherty M, Capewell S, et al. Coronary Heart Disease Mortality Declines in the United States From 1979 Through 2011: Evidence for Stagnation in Young Adults, Especially Women. Circulation. Published September 15, 2015. DOI: 10.1161/CIRCULATIONAHA.115.015293
- Zhao M, Woodward M, Vaartjes I, Millett,ERC, et al. Sex Differences in Cardiovascular Medication Prescription in Primary Care: A Systematic Review and Meta‐Analysis. Journal of the American Heart Association. Published May 20, 2020. DOI: 10.1161/JAHA.119.014742
- Assari S. Veterans and Risk of Heart Disease in the United States: A Cohort with 20 Years of Follow Up. International Journal of Preventative Medicine. Published June 2014. PMCID: PMC4085922
- Vikulova DN, Grubisic M, Zhao Y, Lynch K, et al. Premature Atherosclerotic Cardiovascular Disease: Trends in Incidence, Risk Factors, and Sex-Related Differences, 2000 to 2016. Journal of the American Heart Association. Published July 16, 2019. DOI: 10.1161/JAHA.119.012178
- Okunrintemi V, Valero‐Elizondo J, Patrick B, et al. Gender Differences in Patient‐Reported Outcomes Among Adults With Atherosclerotic Cardiovascular Disease. Journal of the American Heart Association. Published December 10, 2018. DOI: 10.1161/JAHA.118.010498
- Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women Veterans Report: The Past, Present and Future of Women Veterans. Published February 2017.

