ATLANTA—Among veterans, chronic obstructive pulmonary disease, asthma and obstructive sleep apnea all occur at significantly higher rates than in the general population. Greater rates of smoking and obesity contribute to the elevated risk for these conditions in veterans and may drive the relatively high rate at which veterans experience two or more of the conditions simultaneously.
Until recently, though, the impact of having both an obstructive lung disease such as asthma or COPD and obstructive sleep apnea has been poorly understood. And that, it turns out, has some serious implications for veterans.
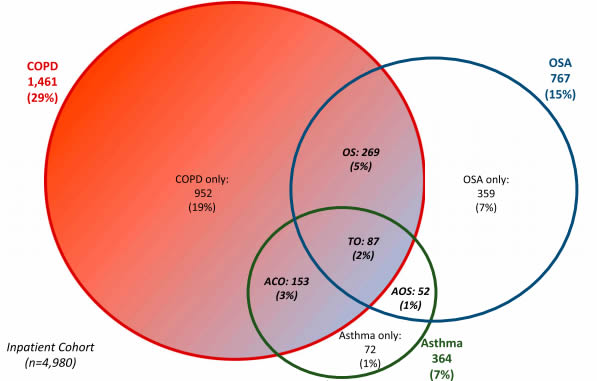
Proportional Venn diagram of the OLDOSA Cohort (n = 4,980). Patient population outside the circles and inside the rectangle is represented by patients with no OSA, COPD, or asthma. Asthma, COPD, and OSA “only” = nonintersecting or nonoverlapping disorders. ACO = asthma and COPD (no sleep apnea), AOS = asthma and OSA (no COPD), COPD = chronic obstructive pulmonary disease, OSA = obstructive sleep apnea, OS = COPD and OSA (no asthma), TO = triple overlap of asthma, COPD and OSA.
The 10-year mortality rate for each disease individually exceeds 50%. Among veterans with comorbid asthma, COPD and OSA, a condition called triple overlap, the rate approaches 70%, according to a recent study published in the Journal of Clinical Sleep Medicine by researchers at the Atlanta VA and Emory University.1
“Assessing long-term outcomes in patients with overlapping conditions such as OLD and OSA is extremely important, for at least a few reasons: these are very common disorders in the general population, long-term control of these diseases is often suboptimal, and the endo-phenotypic classification of OLD is often ‘fuzzy’, while the contribution of these disorders (or their lack of control) to overall survival and long-term morbidity of these individuals is still unclear,” said lead author Octavian C. Ioachimescu, MD, PhD, MBA, medical director of the Sleep Medicine Center and Sleep Medicine section chief at the Atlanta VAMC and professor of medicine at Emory University.
Comorbid Conditions
To better understand the risks and outcomes of each disease and the diseases in combinations, Ioachimescu and his colleagues undertook a 10-year study of veterans in the Atlanta VAMC starting in 2008. Among the 53,123 veterans who had a medical visit to the VAMC that year, 8% had asthma, 14% had sleep apnea, and 19% had COPD. Altogether, one-third of the veterans had at least one of the conditions and 5% had obstructive lung disease (either asthma or COPD) combined with obstructive sleep apnea, or OLDOSA.
The researchers then drilled down further to enable better validation of the records. They identified 4,980 veterans who had been hospitalized at least once in the 2008 calendar year at the Atlanta VAMC, who comprised the OLDOSA cohort. The veterans could have been hospitalized for any reason during 2008 and were not selected specifically for the presence of obstructive lung disease or sleep apnea. All patients in the cohort were followed until death or last visit before one of four data extraction dates in 2016 and 2018.
Veterans in the OLDOSA cohort with obstructive sleep apnea were offered positive airway pressure therapy and education based on clinician recommendations and patient preferences.
Within this cohort that had experienced hospitalization, 7% had a diagnosis of asthma, 15% had OSA, and 29% had COPD, with 39% having at least one of the conditions and 8% having OLDOSA.
Over the 10 years of the study, an additional 702 veterans in this cohort developed obstructive sleep apnea. Of those, 275 had neither of the other conditions, 345 also had COPD, 23 had asthma, and 59 had both. During the study period, 101 additional veterans in the group were diagnosed with asthma and 430 received incident diagnoses of COPD.
Nearly two-thirds of the patients with sleep apnea had started PAP therapy by the end of the study. Of the 536 who had not, the reasons varied from mild disease to patient refusal, failure to attend appointments, or death. As of September 2016, the 238 survivors with OSA who were on PAP therapy used PAP a median of 84.5% of nights for a median of 5.6 hours, with 62% using PAP for at least four hours per night.
Overall, 52.8% of the veterans died during the study, and the median time to death was 2.7 years. Nearly two-thirds of the men in the study died, versus one-third of the women. A number of comorbidities beyond those specifically included in the study boosted death rates to 75% or higher, including congestive heart failure, moderate to severe chronic kidney or liver disease and metastatic solid tumors.
While the overall mortality rate for veterans with COPD was 63%, the rates was considerably higher among those with moderate (71.6%), severe (75%) and very severe airflow limitations (93.5%). Patients with triple overlap had the highest mortality at 67.8%.
PAP Reduces Risk
The researchers determined that use of PAP was particularly important for patients with obstructive sleep apnea in this vulnerable population. Patients with OSA who were not prescribed PAP had a 34% increased risk of death, compared to those who were. Further, patients prescribed PAP therapy who were nonadherent had a 78% increased risk of death compared to those who used it at least 70% of nights for at least four hours per night.
Those findings argue for more frequent recommendations of PAP therapy and greater encouragement and education about the importance of adherence among veterans, according to Ioachimescu.
“The existing data suggest that the COPD-OSA ‘overlap syndrome,’ the asthma-OSA ‘alternative overlap syndrome’ and the ‘triple overlap’ OSA-COPD-asthma would benefit from better adherence to PAP therapy recommendations, perhaps having us reset our treatment plans with a lower threshold to implement motivational enhancement interventions or combined cognitive and behavioral approaches to improve therapeutic compliance,” he noted.
Given the high prevalence of both obstructive lung disease and obstructive sleep apnea, Ioachimescu urged clinicians to look more deeply at the symptoms and possible comorbidities experienced by veterans to improve patient care.
That could enable clinicians “to become better at defining existing OLD and OSA endo-phenotypes,” he said, “which could lead to more personalized therapeutic interventions and better outcome stratification using individual features and available, clinical science-proven, disease characteristics.”
- Ioachimescu OC, Janocko NJ, Ciavatta MM, Howard M, Warnock MV. Obstructive Lung Disease and Obstructive Sleep Apnea (OLDOSA) cohort study: 10-year assessment. J Clin Sleep Med. 2020 Feb 15;16(2):267-277. doi: 10.5664/jcsm.8180.
