Death Pre-Existing CVD Most Risky for Veterans With Virus
INDIANAPOLIS — Strain on intensive care units at the VA during the COVID-19 pandemic appeared to increase patient mortality.
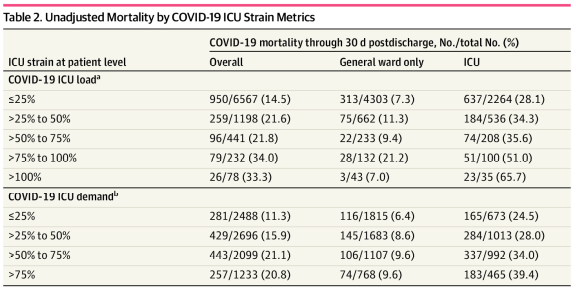
Among 8,516 patients with COVID-19 admitted to 88 VAMCs, those treated in the ICU during periods of peak critical care demand had a nearly twofold increased risk of mortality compared with those treated during periods of low demand, according to a cohort study.
The report in JAMA Network Open said the findings suggest that public health officials and hospital administrators should consider interventions that reduce COVID-19 ICU demand to improve survival rates.1
After nearly a year of U.S. pandemic conditions, that was one of the studies that looked at how the crisis affected VA clinical care. Another looked at which patients were most at risk, finding that veterans 65 and older with a history of heart disease were the most likely to end up in VA hospitals with COVID-19 and also the most likely to die from it during the first few months of the novel coronavirus outbreak.
In the ICU study, the authors from the Richard L. Roudebush VAMC and Indiana University noted that, while strain on hospital capacity has been associated with increased mortality in nonpandemic settings, there was a lack of information on the association between COVID-19 critical care capacity and mortality.
To remedy that, the study team conducted a cohort study among veterans with COVID-19, as confirmed by polymerase chain reaction or antigen testing in the laboratory from March through August 2020. Patients were treated at any VA hospital with 10 or more patients with COVID-19 in the ICU. The follow-up period was through November 2020, with data analyzed from March to November 2020.
Nearly all the participants were men, 94.1%, and had an average age of 67.9. The focus was on treatment for COVID-19 in the ICU during a period of increased COVID-19 ICU load. All-cause mortality was recorded through 30 days after discharge from the hospital.
Results indicated that mortality varied over time, with 218 of 954 patients (22.9%) dying in March, 399 of 1,594 patients (25.0%) dying in April, 143 of 920 patients (15.5) dying in May, 179 of 1,314 patients (13.6%) dying in June, 297 of 2,373 patients (12.5%) dying in July and 174 of 1,361 (12.8%) patients dying in August (P < 0.001).
Researchers also pointed out that COVID-19 patients who were treated in the ICU during periods of increased ICU demand due to the virus had increased risk of mortality compared with patients treated during periods of lower demand, defined as less than 25%. Specifically, they calculated that the adjusted hazard ratio for all-cause mortality was:
- 0.99 (95% CI, 0.81-1.22; P = 0.93) for patients treated when COVID-19 ICU demand was more than 25% to 50%,
- 1.19 (95% CI, 0.95-1.48; P = 0.13) when COVID-19 ICU demand was more than 50% to 75%, and
- 1.94 (95% CI, 1.46-2.59; P < 0.001) when COVID-19 ICU demand was more than 75% to 100%.
Yet, no association between COVID-19 ICU demand and mortality was observed for patients with COVID-19 not admitted to the ICU, the authors noted. Furthermore, they add, the association between COVID-19 ICU load and mortality was not consistent over time, (i.e., early vs. late in the pandemic).
“This cohort study found that, although facilities augmented ICU capacity during the pandemic, strains on critical care capacity were associated with increased COVID-19 ICU mortality,” researchers explained. “Tracking COVID-19 ICU demand may be useful to hospital administrators and health officials as they coordinate COVID-19 admissions across hospitals to optimize outcomes for patients with this illness.”
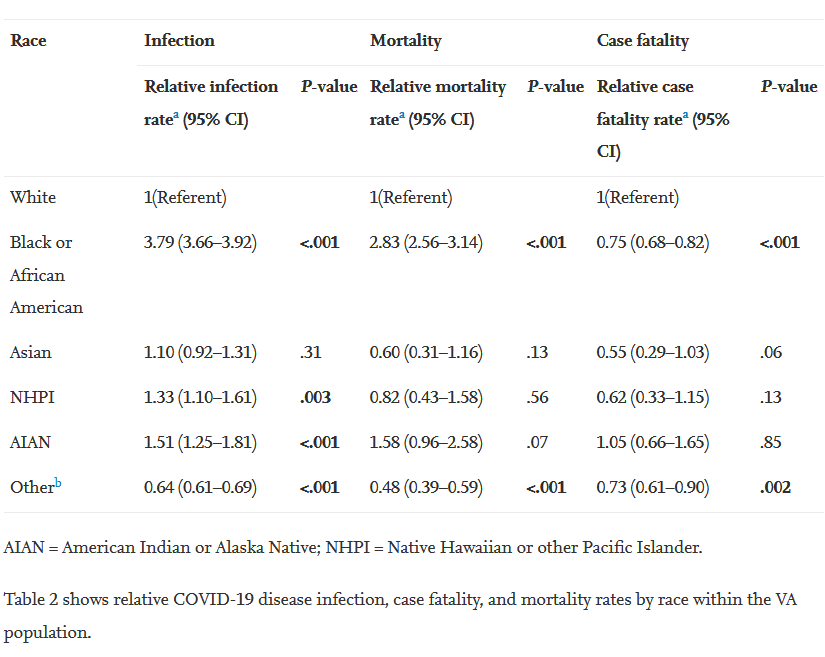
The other study, a report in Annals of Epidemiology, also pointed out that Black veterans had higher mortality rates than white veterans but lower case fatality rates.
The review was conducted by researchers from the George E. Wahlen VAMC and the University of Utah School of Medicine, both in Salt Lake City.
“Veterans represent a significant proportion of the U.S. population (7%), and the impact of the coronavirus disease 2019 (COVID-19) in this group of vulnerable patients has been largely overlooked,” the authors wrote, explaining the need for their study. “This analysis reports COVID-19 patient demographics, infection, mortality, and case-fatality rates in the veteran population.”
The study team used the VA informatics and computing infrastructure tool to assess COVID-19 infections at VAMCs from March 4 to June 3, 2020.
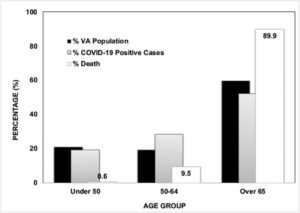
Of the 10,621,580 veterans included in the analysis, 59.7% were 65 or older; 92.5% were men; 68.7% were white; and 14.2% were Black. Results indicated that veterans 65 an older made up 52.1% of cases and 89.9% of deaths. The relative mortality and case-fatality rates of Black veterans, when compared with white veterans, were 2.83 (CI 2.56-3.14; P <0.001) and 0.75 (CI 0.68-0.82; P < 0.001), respectively, the authors pointed out.
In addition, the researchers emphasized that, among the veterans who died from COVID-19, 87.4% had a history of cardiovascular disease, 56.5% had a history of diabetes and 33.6% were obese.
The study noted that veterans are considered a vulnerable population, which the National Collaborating Center for Determinants of Health defines as “groups and communities at a higher risk of poor health as a result of the barriers they experience to social, economic, political, and environmental resources, as well as limitation due to illness or disability.”
“Veterans are more vulnerable and differ from the general public in several ways,” the authors explained. “First, veterans are older, with 50.0% of U.S. veterans ≥65 years, in contrast to 18.5% of civilians. Second, veterans are 14.7 times more likely to be of poor health status and 14 times more likely to have ≥5 medical conditions than the general population. Finally, there are also higher rates of mental health issues among veterans, such as substance use disorder, post-traumatic stress disorder, traumatic brain injuries, depression, suicide, and homelessness.”
The report also advised that veterans who use the VA healthcare system—as opposed to those who receive care elsewhere—are more likely to be from a minority group, less educated, unmarried and have a lower household income, with a higher prevalence of chronic medical conditions.
Different from General Public
The authors, who said their study was the first to analyze the impact of COVID-19 infections and deaths in veterans who have received care at VA facilities, noted that patients at the VA differed from the general public in several ways.
“In this analysis, the highest proportion of veterans with COVID-19 disease was ≥65 years old (52.1%),” they wrote. “This is in contrast to the general population (GP), where the highest proportion with COVID-19 disease is seen in persons 18- 49 years old (50.0%). Possible explanations for this finding are:
- Individuals ≤49 years old constitute a smaller proportion of the total VHA population (21.0%) than in the GP (39.5%);
- Younger veterans are more likely to be covered by private insurance and obtain care at other healthcare facilities;
- Higher rates of testing in the younger civilian population;
- The ≤49 age group represents a substantial proportion of the U.S. workforce, with a limited ability to stay home and more likely to be exposed to the virus.”
Still, the study pointed out, adults 65 and older still make up most COVID-19 deaths in the VHA (89.9%) and the GP (78.6%).
The researchers also commented on possibly confusing statistics affecting Black veterans—a relative mortality rate that was 2.83 times (P <0.001) higher, but a case fatality was 0.75 times (P < 0.001) that of white veterans. “One possible explanation could be that the Black veteran VA utilizers are younger and healthier than white veteran VA-utilizers because the overall U.S. median age for Black veterans is a decade younger than white veterans (55.3 years old vs. 65 years old),” they posited, adding that more research is needed to explain “why Black veterans have a higher rate of COVID-19 infections but experience a lower disease severity”
The study also advised that CVD was the most common comorbid condition seen in both COVID-19 cases (66.6%) and deaths (87.4%) in the VA cohort.
Overall, the authors added, “Of those who tested positive for the COVID-19 disease, the percent of reported deaths in the veteran population is higher than the GP (11.9% vs. 5.2%), as of June 23, 2020 (2). This disparity may be attributed to veterans being older and having a higher prevalence of comorbidities.”
- Bravata DM, Perkins AJ, Myers LJ, et al. Association of Intensive Care Unit Patient Load and Demand With Mortality Rates in US Department of Veterans Affairs Hospitals During the COVID-19 Pandemic. JAMA Netw Open. 2021;4(1):e2034266. doi:10.1001/jamanetworkopen.2020.34266
- Luo J, Jeyapalina S, Stoddard GJ, Kwok AC, Agarwal JP. Coronavirus disease 2019 in veterans receiving care at veteran’s health administration facilities. Ann Epidemiol. 2020 Dec 16;55:10-14. doi: 10.1016/j.annepidem.2020.12.003. Epub ahead of print. PMID: 33338646.