No Racial Disparities Identified, However
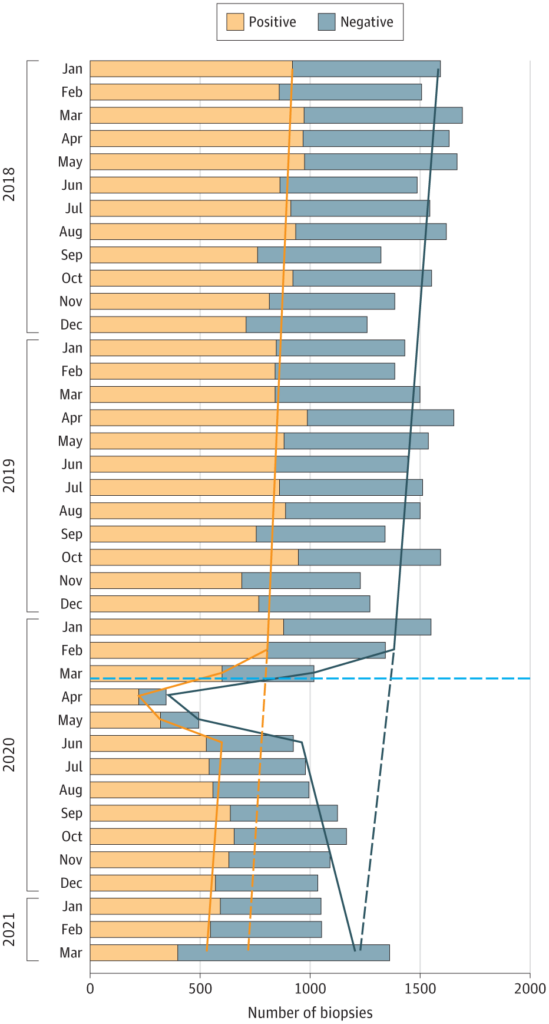
Click to Enlarge: Prostate Biopsies and Newly Diagnosed Cases of Prostate Cancer Stratified by Month Bars represent the observed counts; solid lines represent the expected counts from the interrupted time-series analysis; dashed lines project the expected counts had there not been a COVID-19 pandemic interruption; and the horizontal dashed light blue line indicates March 11, 2020, when the World Health Organization declared COVID-19 a global pandemic. Source:
DURHAM, NC — The COVID-19 pandemic had a negative effect on prostate cancer screening and diagnosis rates among veterans, but no racial discrepancies were identified, according to a new study.
The cohort study, published recently in JAMA Oncology, analyzed all prostate biopsies performed on patients in the entire VA healthcare system without a preexisting prostate cancer diagnosis between January 2018 and March 2021. Preexisting prostate cancer was defined as a diagnosis date more than 30 days prior to a patient’s biopsy date. The study participants included all living male patients who had at least one VHA visit during the three years prior to each month of the study.1
“The study results suggest that prostate biopsy volume and prostate cancer diagnosis rates decreased in the Veterans Affairs Health Care System during the COVID-19 pandemic, with similar declines in both Black and white men,” Stephen Freedland, MD, senior author of the study and a staff physician at the Durham, NC, VAMC , told U.S. Medicine.
“Prior to the pandemic, biopsy rates were statistically significantly higher among Black vs. white men; however, there were no statistically significant changes in biopsy rates associated with race at the onset of the pandemic. In other words, though biopsy rates declined, they declined equally regardless of race,” they said
Using data from a large nationwide equal-access healthcare system, the researchers demonstrated the COVID-19 pandemic was associated with fewer biopsies and fewer new prostate cancer cases, which was particularly pronounced during the pandemic peak.
Before the pandemic (January 2018 through February 2020), monthly biopsy numbers among the 51,606 men included in the study ranged between 1,230 and 1,695, of which 56% to 60% of results were positive for prostate cancer. Among these men, the estimated number of missed prostate cancer diagnoses from March 2020 through March 2021 ranged from 97 to 573 cases per month.
Biopsy Rates
Also, prior to the pandemic, biopsy rates were statistically significantly higher among Black vs. white men (incidence rate ratio, 2.25; 95% CI, 2.06-2.46; P < 0.001). However, there were no statistically significant changes in biopsy rates associated with race at the onset of the pandemic nor during the recovery period from June 2020 through March 2021, with similar trends observed for prostate cancer diagnosis rates, Freedland explained.
The researchers modeled the influence of the pandemic on prostate biopsy volume and the incidence of prostate cancer diagnoses using an interrupted time-series analysis. The models accounted for month-to-month variability in the base population using an offset term for population size and included indicator variables to control for the three months during the peak of the pandemic lockdown. The models also were fitted to evaluate differences in prostate biopsy and prostate cancer diagnosis rates by race (among the subset of Black versus white patients).
“We found that Black men had statistically significantly higher biopsy and prostate cancer diagnosis rates compared with white men prior to the pandemic, with no statistically significant changes by race during the pandemic peak or during the recovery period,” Freedland said in an email. “Importantly, this suggests that Black men did not receive marginalized care relative to white men during the pandemic, perhaps as a result of equal-access care at VA hospitals.”
The study’s results indicate that prostate biopsy volume and prostate cancer diagnosis rates decreased at the VHA during the COVID-19 pandemic, but notably it declined equally in both Black and white men, Freedland said.
“While it was encouraging that the declines were equal by race, there was a little concern that once the restrictions wore off, we saw no evidence of higher than pre-pandemic “make-up” period,” Freedland added. “As a result, the authors concluded that the pandemic has resulted in fewer cancers being diagnosed. What we don’t know is whether these missed cancers were more indolent cancers that probably did not need to be found in the first place or aggressive cancers that will ultimately now be diagnosed at a later stage and will be less curable, leading to an increased risk of prostate cancer death. Ultimately, more follow-up will be needed to assess that.”
This is the first study the researchers are aware of that demonstrates the negative association of the pandemic with cancer screening and diagnosis rates, evaluated by race, in the VA patient population. The data are limited by a lack of information on cancer stage and grade at diagnosis, however, and the authors suggested that the effect of delayed or deferred diagnoses in these men warrants long-term study. Also, because the study was limited to Black and white men, the researchers don’t know if other racial and ethnic groups might have different biopsy or prostate cancer diagnosis trends, the study reported.
Similarly, a 2021 JAMA Oncology study by Bakouny, et al, reported a considerable decrease in screening tests for cancer (mammography, prostate-specific antigen, colonoscopy, Papanicolaou test, low-dose computed tomography) and decreased diagnoses during the pandemic. These studies suggest the pandemic has negatively affected cancer diagnosis rates, regardless of jurisdiction or payment model. Also, COVID-19 variant strains could possibly cause ongoing delays in prostate cancer screening.2
- Klaassen Z, Stock S, Waller J, De Hoedt A, Freedland SJ. Association of the COVID-19 Pandemic With Rates of Prostate Cancer Biopsies and Diagnoses in Black vs White US Veterans. JAMA Oncol. Published online April 07, 2022. doi:10.1001/jamaoncol.2022.0467
- Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh Q. Cancer Screening Tests and Cancer Diagnoses During the COVID-19 Pandemic. JAMA Oncol. 2021;7(3):458–460. doi:10.1001/jamaoncol.2020.7600

