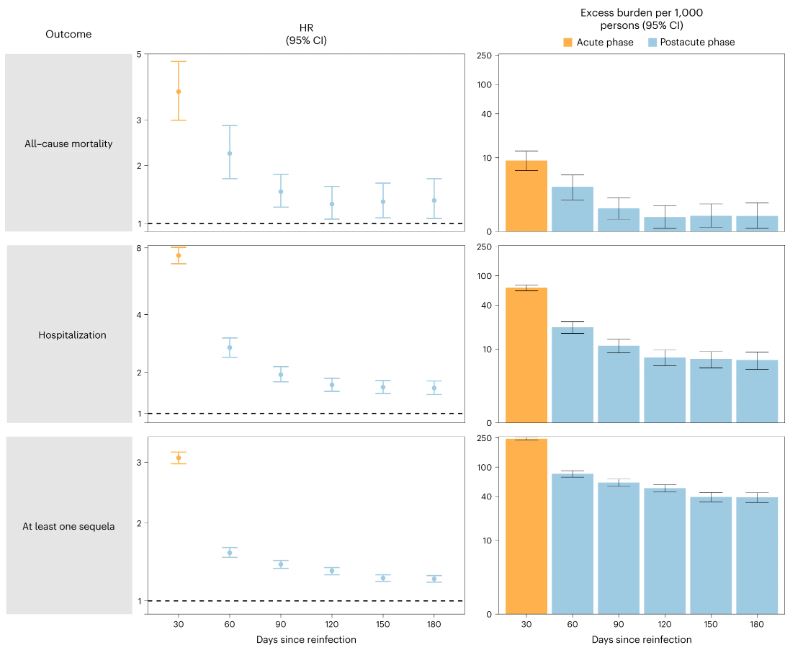
Click to Enlarge: Risk and 6-month burden of all-cause mortality, hospitalization and at least one sequela of SARS-CoV-2 reinfection versus no reinfection in 30-d intervals covering the acute and postacute phases of reinfection. Incident outcomes were assessed from reinfection to the end of the follow-up. Results from SARS-CoV-2 reinfection (n = 40,947) versus first SARS-CoV-2 infection (n = 443,588) by time since reinfection were compared. Adjusted HRs (dots) and 95% CIs (error bars) are presented for each 30-d period since the time of reinfection, as are the estimated excess burden (bars) and 95% CIs (error bars). Burdens are presented per 1,000 persons at every 30-d period of the follow-up from the time of reinfection. Source: Nature Medicine
ST. LOUIS — Despite misconceptions that prior COVID-19 infections can keep patients from having severe cases in the future, a new study suggests that recurrent cases pile on the risk of adverse health conditions in multiple organ systems.
A VA-led study found that reinfected patients were twice as likely to die and three times more likely to be hospitalized. New research suggests those who recovered from past bouts with SARS-C0V-2 should be more, not less, concerned about contracting COVID-19 again.
A study from the VA St. Louis Healthcare System and Washington University School of Medicine in St. Louis revealed the troubling health consequences of reinfection. The findings, published in Nature Medicine, were that repeat SARS-CoV-2 infections contribute significant additional risk of adverse health conditions in multiple organ systems.1
Among those are greater risk of hospitalization; disorders affecting the lungs, heart, brain and the body’s blood, musculoskeletal and gastrointestinal systems; and death. Diabetes, kidney disease and mental health issues also are affected by reinfection.
“During the past few months, there’s been an air of invincibility among people who have had COVID-19 or their vaccinations and boosters, and especially among people who have had an infection and also received vaccines; some people started referring to these individuals as having a sort of super immunity to the virus,” said senior author Ziyad Al-Aly, MD, who is with the VA and Washington University. “Without ambiguity, our research showed that getting an infection a second, third or fourth time contributes to additional health risks in the acute phase, meaning the first 30 days after infection and in the months beyond, meaning the long-COVID phase.”
What are the consequences? “This means that, even if you’ve had two COVID-19 infections, it’s better to avoid a third,” Al-Aly said. “And if you’ve had three infections, it’s best to avoid the fourth.”
The report noted that the first infection with SARS-CoV-2 is linked with an increased risk of acute symptoms, post-acute death and sequelae in various organ systems. The authors said that it had been unclear what effect future infections had.
To answer that question, the study team used the VA’s national healthcare database to build a cohort of 443,588 individuals with one SARS-CoV-2 infection; 40,947 with reinfection, defined as two or more infections; and a non-infected control group of 5.3 million.
Compared to no reinfection, results indicate that reinfection contributed the additional risks of:
- death (hazard ratio (HR) = 2.17, 95% confidence intervals (CI) 1.93-2.45),
- hospitalization (HR = 3.32, 95% CI 3.13-3.51) and
- sequelae including pulmonary, cardiovascular, hematological, diabetes, gastrointestinal, kidney, mental health, musculoskeletal and neurological disorders.
“The risks were evident regardless of vaccination status,” the researchers advised. “The risks were most pronounced in the acute phase but persisted in the post-acute phase at 6 months. Compared to non-infected controls, cumulative risks and burdens of repeat infection increased according to the number of infections.”
They said the research was limited by including a cohort of mostly white males.
Still, the authors added, “Reducing overall burden of death and disease due to SARS-CoV-2 will require strategies for reinfection prevention.”
How to do that? Al-Aly recommended, “People should do their best to prevent repeat infections by masking, for example, getting all of their eligible boosters, staying home when sick. Also, get a flu shot to prevent illness. We really need to do our best to reduce the chance we will have a twin-demic of both COVID-19 and the flu this winter season.”
Overall, the researchers found that people with COVID-19 reinfections were twice as likely to die and three times more likely to be hospitalized than those with no reinfection. They also were 3½ times more likely to develop lung problems, three times more likely to suffer heart conditions and 1.6 times more likely to experience brain conditions than patients who had been infected with the virus only once.
“Our findings have broad public health implications, as they tell us that strategies to prevent or reduce the risk of reinfection should be implemented,” Al-Aly said. “Going into the winter season, people should be aware of the risks and practice vigilance to reduce their risk of infection or reinfection with SARS-CoV-2.”
The authors provided information to help elucidate the cumulative risks incurred by patients with multiple infections. To do that, they estimated the cumulative risk and burden of a set of prespecified outcomes in those who did not have a reinfection, i.e., had one infection, and those who had two or three or more infections during the 1-year period after the acute phase of the first infection, compared to a non-infected control group.
“There was a graded association in that the risks of adverse health outcomes increased as the number of infections increased,” according to the study. “Compared to the non-infected control group, those who only had one infection had an increased risk of at least one sequela (HR = 1.37, 95% CI = 1.36-1.38; burden per 1,000 persons at one-year = 108.88, 95% CI = 105.89-111.87); the risk was higher in those who had two infections (HR = 2.07, 95% CI = 2.03-2.11; burden = 260.41, 95% CI = 253.70-267.09) and highest in those with three or more infections (HR = 2.35, 95% CI = 2.12-2.62; burden = 305.44, 95% CI = 268.07-341.11).”
They added, “In a pairwise comparison of those with two infections versus one infection, those with two infections had an increased risk of at least one sequela (HR = 1.51, 95% CI = 1.48-1.54; burden = 151.53, 95% CI = 144.83-158.21); in pairwise comparison of those with three or more infections versus those with only two infections, those with three or more infections had a higher risk of at least one sequela (HR = 1.14, 95% CI = 1.02-1.27; burden = 45.02, 95% CI = 7.66-80.70). Results were consistent when hospitalization and sequelae by organ system were examined.”
- Bowe, B., Xie, Y. & Al-Aly, Z. Acute and post-acute sequelae associated with SARS-CoV-2 reinfection. Nat Med 28, 2398–2405 (2022). https://doi.org/10.1038/s41591-022-02051-3

