SAN ANTONIO — Is it possible to predict which COVID-19 patients will advance to severe disease? A new study involving VA researchers suggested that the answer is “yes,” using the concept of immunologic resilience.
Researchers from the South Texas Veterans’ Healthcare System and The University of Texas Health Science Center at San Antonio further pointed out that biomarkers tracking immunologic resilience are associated with longevity and also can be used to predict outcomes to other infections such as influenza or HIV.
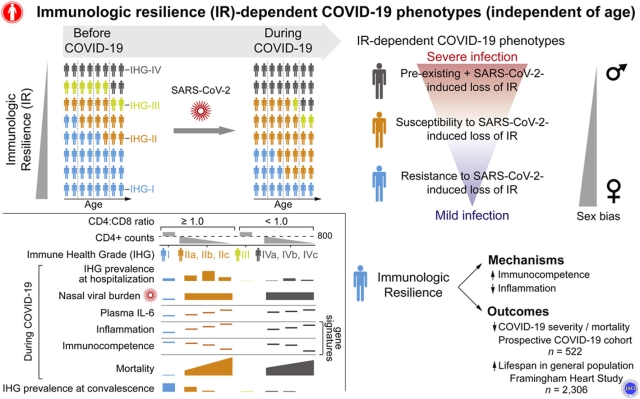
“The risk of severe COVID-19 varies significantly among persons of similar age and is higher in males,” the authors wrote in the Journal of Allergy and Clinical Immunology. “Age-independent, sex-biased differences in susceptibility to severe COVID-19 may be ascribable to deficits in a sexually dimorphic protective attribute that we termed immunologic resilience (IR).”
The study team sought to determine whether mortality from SARS-CoV-2 infection can be predicted by IR that antedates or is induced by SARS-CoV-2 infection independently.
To do that, researchers quantified IR levels with two metrics: immune health grades (IHG-I [best] to IHG-IV) to gauge CD8+ and CD4+ T-cell count equilibrium, and blood gene expression signatures. Those metrics were used in in a prospective COVID-19 cohort of 522 people, with the primary outcome defined as 30-day mortality.
They noted that associations of IR metrics with outcomes in non-COVID-19 cohorts involving 13,461 participants were used link pre-COVID-19 IR status to IR during active infection and outcomes.
Results indicated that “IHG-I, tracking high-grade equilibrium between CD8+ and CD4+ T-cell counts, was the most common grade (73%) among healthy adults, particularly in females,” the authors reported. “SARS-CoV-2 infection associated with underrepresentation of IHG-I (21%) vs. overrepresentation (77%) of IHG-II or IHG-IV, especially in males vs. females (P<0.01).”
In fact, the researchers advised that T cell equilibrium was associated with 88% lower mortality, after controlling for age and sex. Having better immunologic resilience also reduced risk of hospitalization and respiratory failure, they added, noting that lower plasma IL-6 levels; rapid clearance of nasopharyngeal SARS-CoV-2 burden; and gene expression signatures correlated “with survival that signify immunocompetence and controlled inflammation.”
In those without COVID-19, the study team revealed that iIR-preserving metrics were associated with resistance to progressive influenza or HIV infection, as well as lower nine-year mortality in the Framingham Heart Study, especially in females.
“Preservation of immunocompetence with controlled inflammation during antigenic challenges is a hallmark of IR and associates with longevity and AIDS resistance,” the researchers concluded. “Independent of age, a male-biased proclivity to degrade IR before and/or during SARS-CoV-2 infection predisposes to severe COVID-19.”
For the research, every COVID-19 patient treated at the Audie L. Murphy Memorial VAMC had immunologic resilience assessed. Each patient’s level of immunological resilience was assessed on the day of admission and then daily for varying durations. Patients whose infections did not require hospital admission were visited at home for assessments. For comparative purposes, the researchers evaluated metrics of immunologic resilience in 13,461 individuals without COVID-19.
Veterans’ IR Measured
“When the pandemic began, it became obvious that it would be very important for us to assess immune status from the day a patient is admitted all the way through the convalescence phase,” explained first author Grace C. Lee, PharmD, PhD, assistant professor, UT Health Science Center San Antonio and The University of Texas at Austin College of Pharmacy, and senior translational research scientist with the Foundation for Advancing Veterans’ Health Research. “We applied these immune metrics to every COVID-19 patient who came into the VA hospital. These metrics are highly prognostic. Metrics tracking inferior immunologic resilience predicted up to 19-times higher risk of dying within 30 days, which was the primary outcome of the study.
She pointed out that the results provide clues to why men fared so much worse during the COVID-19 pandemic, stating, “Remarkably, irrespective of their COVID-19 status, men have inferior immunologic resilience, which may explain why they are predisposed to worse COVID-19 outcomes.”
The authors emphasized that immunologic resilience is not solely related to age, although the proportion of individuals with capacity to preserve immunologic resilience declines, contributing to the greater burden of COVID-19 in older persons. Researchers also suggested that vaccines might be less durable in patients with inferior immunologic resilience.
“One reason this is important is that we are measuring immunologic resilience on the first day, before the patients receive therapy,” said co-first author Marcos Restrepo, MD, MSc, PhD, professor of medicine at the health science center and director of the medical intensive care unit in the South Texas Veterans Health Care System, “Moreover, the failure to show improvements in metrics of immunologic resilience during hospitalization is a prognosticator of worse outcomes.”
One result was an improved ability to determine which patients might need greater interventions to survive novel coronavirus infection. “The concept is a useful way to assess the severity levels of patients and understand their potential rate of progression and need for advanced therapies and longer hospitalizations,” said co-author Sandra Sanchez-Reilly, MD, professor of medicine at the health science center and associate chief of service for geriatrics and extended care in the South Texas Veterans Health Care System.
The authors said the study had some limitations, including that the COVID-19 patients included mostly male U.S. veterans, many of whom were older and had other conditions, such as high blood pressure or diabetes.
- Lee GC, Restrepo MI, Harper N, Manoharan MS, et. al. Immunologic resilience and COVID-19 survival advantage. J Allergy Clin Immunol. 2021 Sep 8:S0091-6749(21)01363-4. doi: 10.1016/j.jaci.2021.08.021. Epub ahead of print. PMID: 34508765; PMCID: PMC8425719.