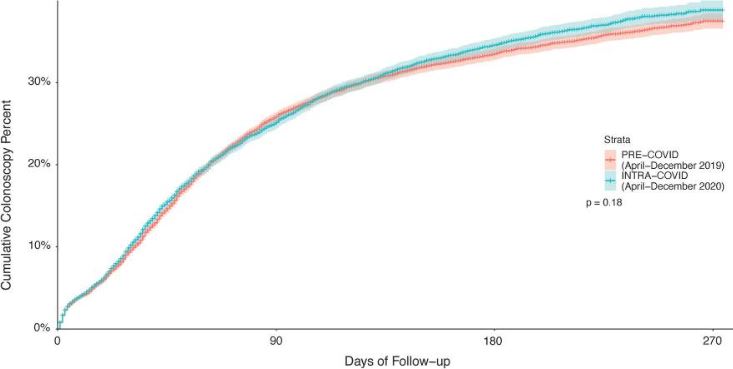
Click to Enlarge: Cumulative colonoscopy completion in a national sample of US Veterans with red flag signs and symptoms of CRC pre- vs. intra-COVID-19 pandemic. Survival curves, estimated via Kaplan–Meier approach for the outcome of time to colonoscopy completion, are shown for individuals with red flag signs or symptoms pre- vs. intra-COVID-19 pandemic. The curves demonstrate a similar cumulative proportion with colonoscopy completion for individuals with red flag signs/symptoms post vs. pre-COVID-19 pandemic. Red flags included abnormal FIT/gFOBT, iron deficiency anemia, and hematochezia. Source: Digestive Diseases and Sciences
SAN DIEGO — Concerns have been raised over the past few years that, because of the COVID-19 pandemic, VHA patients with “red flag signs or symptoms” of colorectal cancer (CRC) did not receive prompt colonoscopy workups.
A study led by researchers from the VA San Diego Healthcare System and University of California, San Diego, sought to find out if that had indeed occurred. Their results, which compared colonoscopy uptake and time to colonoscopy after red flag diagnosis, before and during the COVID-19 pandemic, were published in Digestive Diseases & Sciences.1
The cohort study involved VHA patients ages 50-75 with iron deficiency anemia (IDA), hematochezia, or abnormal stool blood tests from April 2019 to December 2020. Considered the index date was the first red flag diagnosis date. The cases were categorized as “pre” (April-December 2019) and “intra” (April-December 2020) policy implementation which prioritized diagnostic procedures, allowing for a 3-month “washout” (January-March 2020) period.
The study team focused on colonoscopy completion and time to colonoscopy pre- vs. intra-COVID-19 in 52,539 veterans with red flag signs or symptoms—pre-COVID: 25,154; washout: 7527; intra-COVID: 19,858.
Results indicated that the proportion completing colonoscopy was similar pre- vs. intra-COVID-19 (27.0% vs. 26.5%; p = 0.24). In addition, the median time to colonoscopy among colonoscopy completers was found to be similar for pre- vs. intra-COVID-19 (46 vs. 42 days), but longer for individuals with IDA (60 vs. 49 days). No association between time period and colonoscopy completion (aHR: 0.99, 95% CI 0.95-1.03) was identified, the researchers reported.
“Colonoscopy work-up of CRC red flag signs and symptoms was not delayed within VHA during the COVID-19 pandemic, possibly due to VHA policies supporting prioritization and completion”, the authors concluded. “Further work is needed to understand how COVID-19 policies on screening and surveillance impact CRC-related outcomes, and how to optimize colonoscopy completion after a red flag diagnosis.”
Background information in the article recounted how VHA postponed all non-urgent medical procedures to limit transmission and preserve personal protective equipment (PPE), personnel and other hospital resources. That included postponement and re-prioritization of endoscopic procedures, including screening, surveillance and diagnostic colonoscopies.
“VHA facilities were directed to cease all non-urgent and elective procedures no later than March 18, 2020, with additional guidance for primary care providers to order colorectal (CRC) screening with fecal immunochemical tests (FIT), instead of average-risk screening colonoscopy,” the study noted, adding that, on April 2, 2020, VHA provided guidance for prioritization of gastrointestinal (GI) endoscopic consults.
Toolbox Implemented
“To facilitate documentation of priorities as part of the usual workflow for triage of procedure referrals, a “Consult Prioritization Toolbox” was implemented on April 20, 2020, at all VHA locations,” the researchers advised. “This toolbox was embedded within the electronic health record (EHR) and allowed discrete selection of priority categories as part of routine review of consults for procedures.”
Based on guidance from the National GI and Hepatology program, patients were stratified into four groups:
- Priority 1, indications for urgent procedures performed despite the COVID-19 pandemic;
- Priority 2, non-urgent procedures performed as soon as non-urgent procedures could be scheduled;
- Priority 3, routine cases more time sensitive than Priority 4; and
- Priority 4, routine cases that were not particularly time sensitive.
The study authors pointed out that examples of priority assignment included GI bleeding with symptoms and FIT-positive for 3 months or more to Priority 1, stable iron deficiency anemia (IDA) without symptoms and esophageal variceal banding to Priority 2, screening colonoscopy for persons at high risk for CRC and chronic diarrhea without “red flag” symptoms to Priority 3, and average-risk screening colonoscopy and endoscopic surveillance of pancreatic cysts to Priority 4.
In May 2020, HA provided additional guidance on how and when to resume endoscopic procedures deemed non-urgent or elective.
“Throughout the pandemic, individual VHA sites had discretion to increase or decrease procedure access based on local issues, including COVID-19 incidence, availability of SARS-CoV-2 testing and PPE, and staffing,” according to the report. “These postponements had potential to significantly impact diagnostic work-up of persons presenting with CRC red flag signs or symptoms (signs/symptoms), including abnormal FIT or guaiac fecal occult blood test (gFOBT), IDA, or hematochezia.”
They added that, even before the pandemic, studies found that longer wait times from abnormal FIT/gFOBT tests or new symptom onset to diagnostic tests could lead to adverse cancer outcomes. “Although the COVID-19 pandemic has been associated with dramatic disruptions of healthcare delivery and postponement of elective and non-urgent procedures, this study of a national sample of adults with CRC red flag signs/symptoms demonstrated no clinically meaningful change in colonoscopy completion compared to a representative pre-pandemic time period. Moreover, the colonoscopy completion rates of 27.0% and 26.5% in the pre-and intra-COVID-19 periods, respectively, reflect soberingly low diagnostic work-up rates after identification of red flag signs/symptoms.”
In fact, the study team found that the time to colonoscopy was shorter among veterans with IDA during the intra-COVID-19 period.
“Interestingly, time to colonoscopy completion stood out as markedly longer in the pre-COVID-19 period (median 57 days) compared to the intra-COVID-19 period (median 49 days) for patients with IDA,” the authors noted. “We postulate this is because of variation among clinicians in the knowledge that about 9% of individuals with IDA have CRC, and that assignment of IDA as a Priority 2 condition reduced the impact of this variation in knowledge on recommendations and scheduling for colonoscopy. As such, this observed outcome may suggest that providing scheduling priority guidance for common GI disease signs and symptoms, based on available literature on factors such as prevalence of malignancy or likelihood of needing immediate medical management, could improve timely diagnosis and treatment of individuals based on their disease risk.”
Overall, the findings suggested that colonoscopy uptake and timeliness among veterans with CRC red flag signs/symptoms were not significantly impacted, even though, in July 2020, the VA published findings showing colonoscopy volume decreases of 42% and 93% for March and April 2020, respectively.
“Despite the significant drop in overall endoscopy volume for procedures with any indication described in that study, our findings indicate that colonoscopy uptake and time to colonoscopy were preserved among individuals needing diagnostic work-up for CRC red flag signs/symptoms,” the researchers wrote.
They added, “Though the pandemic continues, evidence from our study indicates that, despite VHA recommendations to postpone and re-prioritize colonoscopies at the start of the pandemic, colonoscopy completion, and time to colonoscopy were preserved, and for some indications, improved, compared to the pre-pandemic timeframe among adults with select CRC red flag signs/symptoms. Our findings support the potential utility of prioritization strategies for endoscopy referral which were implemented during the pandemic by VHA, both in regular practice and during future pandemics.”
The authors called for future studies to examine “whether diagnostic yield and CRC outcomes, such as stage at diagnosis or CRC-related mortality, differed pre- vs. post-COVID-19 related to these postponements and if certain colonoscopy prioritization strategies could be more broadly effective in diverse healthcare settings, as we continue to optimize care during and beyond the COVID-19 pandemic.”
- Demb J, Liu L, Bustamante R, Dominitz JA, et. al. COVID-19 Pandemic Had Minimal Impact on Colonoscopy Completion After Colorectal Cancer Red Flag Sign or Symptoms in US Veterans. Dig Dis Sci. 2022 Sep 28:1–10. doi: 10.1007/s10620-022-07685-4. Epub ahead of print. PMID: 36169748; PMCID: PMC9516530

