Rate Considered Low But ‘Not Insignificant’
By: Celeste E. Whittaker
PITTSBURGH — More than 144 million people in the United States had been fully vaccinated against COVID-19 by mid-June, according to the national Centers for Disease Control and Prevention. Yet, while the vaccines work extremely well, nothing is 100% effective, so breakthrough cases are expected, public health officials emphasized.
A vaccine breakthrough infection is defined as the detection of SARS-CoV-2 RNA or antigen in a respiratory specimen collected from a person more than 14 days after they have completed all recommended doses of a U.S. Food and Drug Administration (FDA)-authorized COVID-19 vaccine, the CDC explained.
A new veterans’ study published as a letter in the Journal of Infection provided more information on breakthrough infections in the nation’s largest healthcare system.
VA Pittsburgh Healthcare System-led researchers focused on 58,716 fully vaccinated veterans and identified 410 of those with breakthrough infections and 14,465 controls. The study data set identified all veterans who received two doses of the Pfizer-BNT-162b2 or Moderna-mRNA-1273 vaccine between Dec. 15, 2020 and March 31, 2021. The study was supported by data created by the national VA COVID-19 Shared Data Resource, the authors said.
Excluded from the study were patients with a positive SARS-CoV-2 PCR on a nasopharyngeal swab within 14 days of receiving the first vaccine dose and “from the remaining persons, they retained those who had at least one SARS-CoV-2 PCR test performed on a nasopharyngeal swab more than seven days after the second dose vaccine dose,” according to the report.
“Recently available data from other groups also confirms very high levels of effectiveness of the Pfizer-BNT-162b2 vaccine in the real-world settings,” the authors wrote, adding, “Despite such high efficacy and effectiveness, there are anecdotal reports of breakthrough infection among vaccine recipients. Clinical characteristics and risk factors for SARS-CoV-2 infection after a full recommended course of vaccination is not known. We report the rate and risk factors associated with infection among U.S. veterans who received a recommended course of vaccination.”
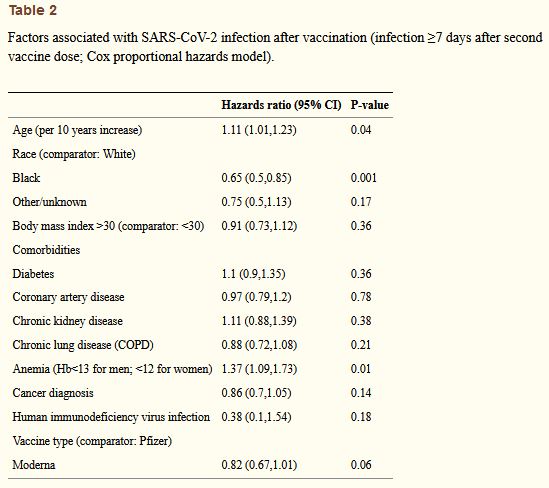
In terms of demographics, the median age was 73 years for the infected group and 72 for the uninfected group. In addition, the study showed there were more whites in the infected group—76.6% to 69.1%—compared to the uninfected and the prevalence of comorbidities was similar in the two groups, except anemia, which was more common in the infected group.
The overall infection rate more than seven days after the second vaccine dose was 0.66 per 1000 person-days of follow-up, with rates not found to be statistically significantly different by age group, sex or the type of vaccine administered. The rate was lower, however, among Blacks compared to whites (0.49 vs. 0.73 per 1,000 person-years) and among those with no comorbidities (0.44) compared with those with one to three comorbidities (0.68).
“Surprisingly, Black race was associated with a lower risk of infection,” the authors pointed out. “… It is possible that the Blacks who were vaccinated were younger and healthier and at a lower risk of infection at the outset. It is equally possible that they were older and less healthy and, due to those reasons, they were less mobile and therefore less likely to be exposed to persons with confirmed infection. Further studies are warranted to confirm this finding and to understand the reasons for this finding.”
Researchers added that their study had several strengths, including that they included a national population with diverse geographical and demographic characteristics who receive care within a single integrated healthcare network. They emphasized that vaccines, SARS-CoV-2 testing and clinical care are provided free or with minimal expense to qualified veterans.
On the other hand, they noted that veterans are predominantly male and that the study “The VA created a national database of SARS-CoV-2 infected veterans using validated did not look at the actual exposure to confirmed cases nor did it focus on clinical severity of disease or outcomes in the study subjects.
The authors concluded that the rate of infection among fully vaccinated persons is low “but not insignificant. Increasing age and presence of anemia increase the risk, while Black race is associated with a lower risk. An awareness campaign, particularly targeted to those at risk is needed to mitigate the risk.”
The CDC announced recently that it planned only to monitor breakthrough infections that result in hospitalization or death, a shift from its previous efforts to track all breakthrough cases.
Army Lt. Gen. Ronald Place, director of the Defense Health Agency, told reporters in May that DoD had tracked about 1,650 “breakthrough” infections in beneficiaries who have been fully vaccinated. While there had been two-dozen hospitalizations, no deaths occurred, he said.
At that time, he said, more than 1.5 million people within the DoD fully had been fully vaccinated. The DoD activated a COVID-19 registry about a year ago, Place said, and tracks issues with its beneficiaries, including breakthrough cases.
“And we also have the same sort of database for everybody that we vaccinated,” he said. “So even though the CDC isn’t requiring it, we still track it.”
Also, he said, “The good news to all is that—as opposed to the 95 percent or whatever rates that we’re seeing published from the phase 2 or phase 3 clinical trials—if you do that math, 99.9 percent effective for our beneficiaries of preventing breakthrough infection, and 99.999 percent effective in preventing hospitalization and 100 percent in preventing death.”
- Butt AA, Khan T, Yan P, Shaikh OS, Omer SB, Mayr F. Rate and risk factors for breakthrough SARS-CoV-2 infection after vaccination. J Infect. 2021 May 28:S0163-4453(21)00263-2. doi: 10.1016/j.jinf.2021.05.021. Epub ahead of print. PMID: 34052241; PMCID: PMC8159711.