
Ziyad Al-Aly, MD, of the VA St. Louis Healthcare System and Washington University School of Medicine. Press release photo by Matt Miller of Washington University.
ST. LOUIS — Survivors of COVID-19 are at heightened risk of developing gastrointestinal (GI) disorders within a year after infection compared with those who were never infected, according to a new study of veterans being treated by the VHA.
Researchers from Washington University School of Medicine in St. Louis and the VA St. Louis Health Care system point out that those conditions can include liver problems, acute pancreatitis, irritable bowel syndrome, acid reflux and ulcers in the lining of the stomach or upper intestine. Post-COVID-19, those patients also have an increased likelihood of constipation, diarrhea, abdominal pain, bloating and vomiting, according to the report in Nature Communications.1
“Gastrointestinal problems were among the first that were reported by the patient community,” said senior author Ziyad Al-Aly, MD, a VA clinical epidemiologist who has studied extensively the long-term effects of COVID-19 infection. “It is increasingly clear that the GI tract serves as a reservoir for the virus.”
The study team used the VA’s national healthcare databases to build a cohort of 154,068 veterans with COVID-19, 5,638,795 contemporary controls and 5,859,621 historical controls to estimate the risks and 1-year burdens of a set of prespecified incident gastrointestinal outcomes.
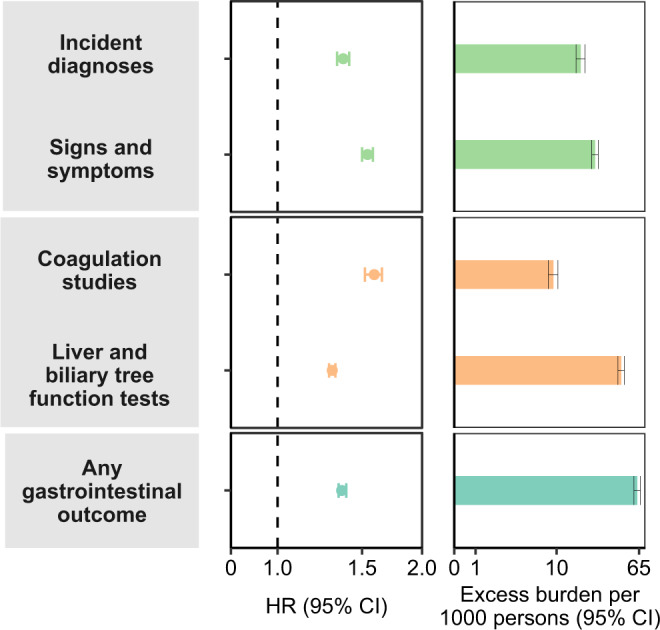
Click to Enlarge: Risks and 1-year burdens of incident post-acute COVID-19 composite gastrointestinal outcomes compared with the contemporary control cohort.
Composite outcomes consisted of incident diagnoses (GERD, PUD, acute pancreatitis, functional dyspepsia, acute gastritis, IBS, and cholangitis), signs and symptoms (constipation, abdominal pain, diarrhea, vomiting, and bloating), coagulation studies (PT, PTT, INR), liver and biliary tree function tests (albumin, ALT, total protein, AST, LDH, CRP, ALP, total bilirubin, GGT, direct bilirubin, lipase, and amylase) and any gastrointestinal outcome (incident occurrence of any gastrointestinal outcome studied). Outcomes were ascertained 30d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 154,068) and contemporary control cohort (n = 5,638,795). Adjusted HRs (dots) and 95% (error bars) CIs are presented, as are estimated excess burdens (bars) and 95% CIs (error bars). Burdens are presented per 1000 persons at 12 months of follow up. The dashed line marks an HR of 1.00; lower limits of 95% CIs with values greater than 1.00 indicate significantly increased risk. GERD gastroesophageal reflux disorder, IBS irritable bowel syndrome, PT prothrombin time, PTT partial thromboplastin time, INR international normalized ratio, ALT alanine transaminase, AST aspartate transaminase, LDH lactate dehydrogenase, CRP c-reactive peptide, ALP alkaline phosphatase, GGT γ-glutamyl transferase. Source: Nature Communications
“We show that beyond the first 30 days of infection, people with COVID-19 exhibited increased risks and 1-year burdens of incident gastrointestinal disorders spanning several disease categories including motility disorders, acid related disorders (dyspepsia, gastroesophageal reflux disease, peptic ulcer disease), functional intestinal disorders, acute pancreatitis, hepatic and biliary disease,” the researchers advised. “The risks were evident in people who were not hospitalized during the acute phase of COVID-19 and increased in a graded fashion across the severity spectrum of the acute phase of COVID-19 (non-hospitalized, hospitalized, and admitted to intensive care).”
While it is increasingly understood that SARS-CoV-2 infection can lead to a range of post-acute sequelae, called long COVID, which can involve the pulmonary and several extrapulmonary organs including the gastrointestinal system, a comprehensive evaluation of the risks and burdens of gastrointestinal disorders in the post-acute phase of COVID-19 had not been conducted prior to this study.
“The constellation of findings suggests that people with SARS-CoV-2 infection are at increased risk of gastrointestinal disorders in the post-acute phase of COVID-19,” the authors wrote. “The risks and burdens are not trivial—suggesting that post-acute COVID care strategies should include attention to gastrointestinal disease.”
The researchers noted that the absolute burdens might appear to be slight, “because of the large number of people with SARS-CoV-2 infection, these rates may translate into large number of affected people. This will have ramifications not only for the personal health of affected individuals, but also on health systems, which will have to address the care needs of people with post-acute COVID-19 gastrointestinal disorders.”
They also pointed out that, while vaccines reduce the risk, they don’t completely abrogate the threat of post-acute sequelae. Reinfection, even in those who were vaccinated, adds to the danger, according to the authors.
Post-Acute Sequelae
“Altogether, the evidence base reinforces the need for continued emphasis on primary prevention of SARS-CoV-2 infection (and prevention of reinfection) as the foundation of the public health response,” according to the study. “Woven together with the evidence amassed thus far on the scale and breadth of organ dysfunction in long COVID, the findings in this report call for the urgent need to develop strategies to prevent and treat the post-acute sequelae of SARS-CoV-2 infection.”
The study team posited several theories about why gastrointestinal and other manifestations of long COVID are occurring. Those include intestinal microbiome dysbiosis, persistence of the virus in immune privileged sites and subsequent chronic inflammation that might provoke organ injury, autoimmune mechanisms and tissue injury during the acute phase, which lead to clinical sequelae in the post-acute phase of the disease.
The findings related to gastrointestinal effects of long COVID follow previous Al-Aly research on lasting effects on the brain, heart, kidneys and other organs.
“At this point in our research, the findings on the GI tract and long COVID did not surprise us,” Al-Aly said. “The virus can be destructive, even among those considered healthy or who have had mild infections. We’re seeing COVID-19’s ability to attack any organ system in the body, sometimes with serious long-term consequences, including death.”
The researchers estimated that, at this point, infections caused by SARS-CoV-2 have contributed to more than 6 million new cases of GI disorders in the U.S. and 42 million new cases worldwide.
“This is no small number,” said Al-Aly, who treats patients within the VA St. Louis Health Care System and is its chief of research and development service. “It is crucial to include GI health as an integral part of post-acute COVID care.”
Overall, GI disorders were 36% more likely in people with COVID-19 compared with those who had not been infected with the virus. This includes people who were and were not hospitalized because of the virus.
While veterans in the study were mostly older white men, the researchers also analyzed data that included more than 1.1 million women and adults of all ages and races. “Those who acquired long-term GI problems after infection included people of all ages, sexes and racial backgrounds,” Al-Aly emphasized.
Compared with patients in the control groups, COVID-19 survivors were found to be at a 62% increased risk of developing ulcers in the lining of the stomach or small intestine; a 35% heightened risk of suffering from acid reflux disease; and a 46% increased risk of experiencing acute pancreatitis.
Those veterans who previously had been infected with the SARs-C0V-2 virus also were 54% more likely to suffer from irritable bowel syndrome, 47% more likely to experience inflammation of the stomach lining, and 36% more likely to have an upset stomach without an obvious cause. Digestive symptoms such as constipation, diarrhea, bloating, vomiting and abdominal pain were 54% more likely.
“Taken with all the evidence that has accumulated thus far, the findings in this report call for the urgent need to double down and accelerate our effort to develop strategies to prevent and treat the long-term health effects after COVID-19 infection,” Al-Aly said.
- Xu E, Xie Y, Al-Aly Z. Long-term gastrointestinal outcomes of COVID-19. Nat Commun. 2023 Mar 7;14(1):983. doi: 10.1038/s41467-023-36223-7. PMID: 36882400; PMCID: PMC9992516.
