BMI’s Role
BMI played a small role in mediating the association, but “it remains unclear whether weight change is a true mediator or a marker of other illness,” the authors said.
On average, the population taking insulin gained more weight than those on sulfonylureas, with a change in BMI or 0.36 kg/m2 compared to 0.26 kg/m2 over 12 months. While some patients gained a significant amount of weight, others lost weight. “Those who lost weight may have had an underlying condition or frailty that affected the provider choice of insulin,” Roumie noted.
Overall, the “study suggests that changes in BMI or hypoglycemia were probably not the key mechanisms that explain the higher risk of death among metformin users adding insulin versus sulfonylurea,” they wrote.
The retrospective study included veterans who intensified therapy for at least 12 months. Of the 28,892 who survived for the full year, 27,239 added a sulfonylurea, and 1,653 added insulin to metformin. Patients were 96% male and 83% white, with a median age of 61 years.
A propensity score weighted cohort of 3,219 veterans split between the two therapies was used for analysis. In the weighted model, the rate of all-cause death per 1,000 per years was 15.4 in the group that added insulin and 12.9 in the sulfonylurea group.
Despite the increase in the risk of death found in the study, providers may still prefer to prescribe insulin over sulfonylureas for a number of reasons.
“Insulin provides fast and flexible blood sugar coverage. Patients may not be candidates for oral medications. Certain comorbidities restrict use of sulfonylureas. Patients may have reduced kidney function, and a physician typically wouldn’t want to use oral sulfonylureas because they stay in the system longer and can have more consequences,” Roumie explained. Perhaps most important, “insulin is very effective at lowering blood glucose and both dose and timing of dose can be tailored to the individual patients.”
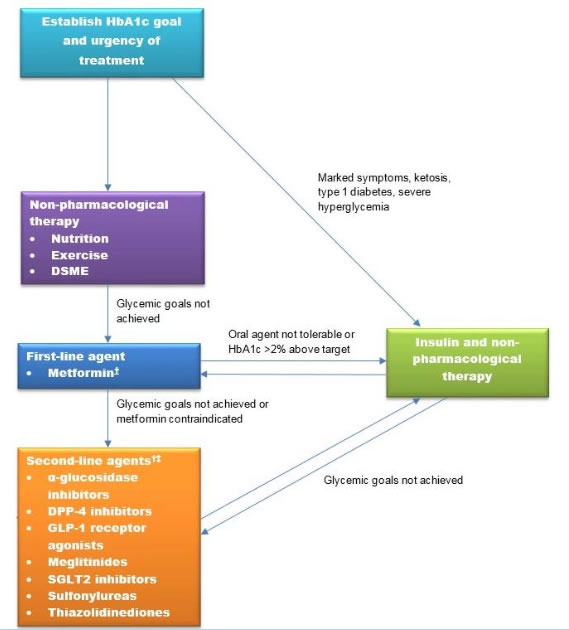
Sulfonylureas also suffer from a lingering public relations problem. “A lot of guidance has veered away from sulfonylureas. The history goes back more than 50 years to a very old university trial that found some increased risk from use of a first-generation sulfonylurea,” she said. A study published in September by Roumie and her colleagues found no harmful effects of sulfonylureas compared to inhibitors of dipeptidyl peptidase 4 (DPP-4 inhibitors or gliptins), which many endocrinologists favor because they are cardiac neutral.
The bigger issue for Roumie is not whether a provider should recommend sulfonylurea or insulin. It’s whether a patient needs anything more than metformin.
“Many patients are still treated too aggressively, despite their age and comorbidities,” she said. “VA/DoD guidelines ask physicians to assess patient risk of treatment and customize therapy based on their comorbidities, life expectancy and shared decision-making with the patient. For many older patients, an A1c of 8% to 9% is completely appropriate.
- Min JY, Hackstadt AJ, Griffin MR, Greevy RA Jr, Chipman J, Grijalva CG, Hung AM, Roumie CL. Evaluation of weight change and hypoglycaemia as mediators in the association between insulin use and death. Diabetes Obes Metab. 2019 Aug 2. doi: 10.1111/dom.13846. [Epub ahead of print]