White T2D Patients More Likely to Get Them; Is Racism the Issue?
SAN FRANCISCO ― Even though novel therapies for type 2 diabetes have been proven to reduce the risk of cardiovascular disease and chronic kidney disease progression, VHA prescription rates remain low. And, compared with white veterans, those of all other racial groups had significantly lower odds of prescriptions for sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA), with Hispanic patients the least likely.
That’s according to a new study in JAMA looking at prescription equitability among more than 1 million patients with type 2 diabetes. The cross-sectional analysis used data from the VHA’s Corporate Data Warehouse. Included in the study were adult patients with type 2 diabetes and at least two primary care clinic visits, from Jan. 1, 2019, to Dec.r 31, 2020.
Researchers from the University of California, San Francisco and the San Francisco VA Healthcare System defined the primary outcomes as any active SGLT2i or GLP-1 RA prescription during the study period.
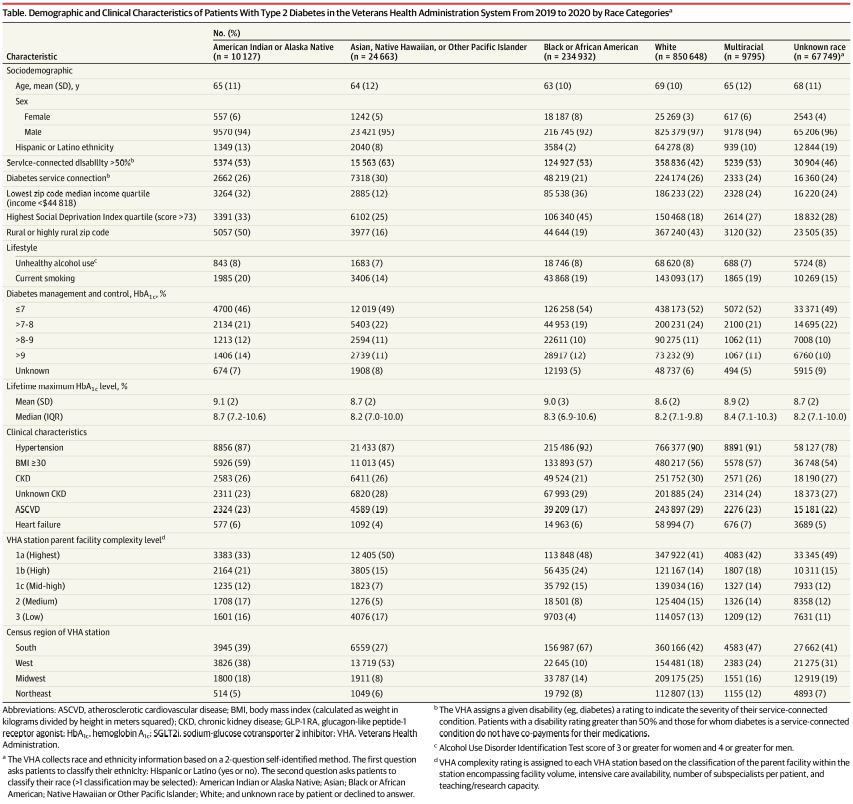
The 1.2 million VHA patients, 96% men, had a mean age of 68 years. The racial/ethnic breakdown was:
- 1% American Indian or Alaska Native,
- 2% Asian, Native Hawaiian, or Other Pacific Islander,
- 7% of Hispanic or Latino,
- 20% Black or African American, and
- 71% white.
During the study period, only 10.7% and 7.7% were prescribed an SGLT2i or a GLP-1 RA, respectively. Researchers reported that prescription rates for SGLT2i and GLP-1 RA, respectively, were 11% and 8.4% among American Indian or Alaska Native patients; 11.8% and 8% among Asian, Native Hawaiian, or Other Pacific Islander patients; 8.8% and 6.1% among Black or African American patients; and 11.3% and 8.2% among White patients, respectively.
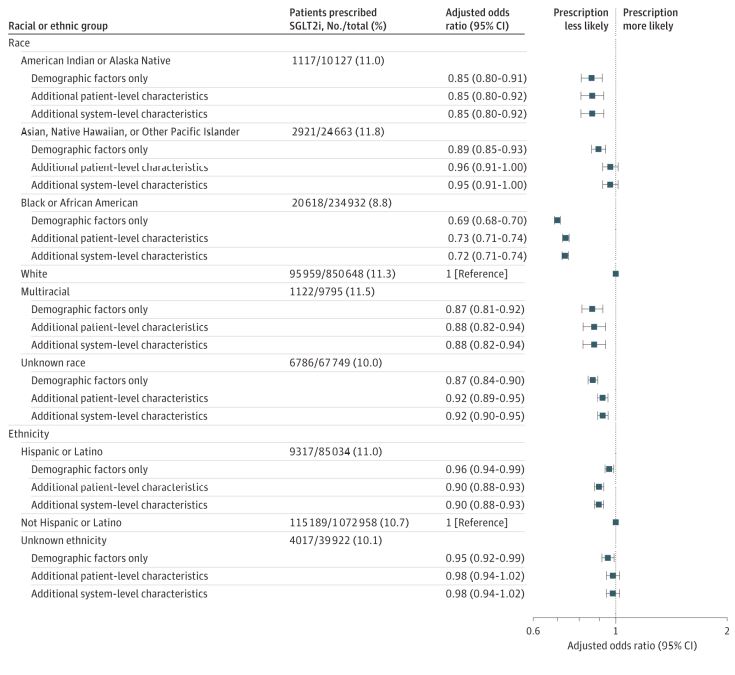
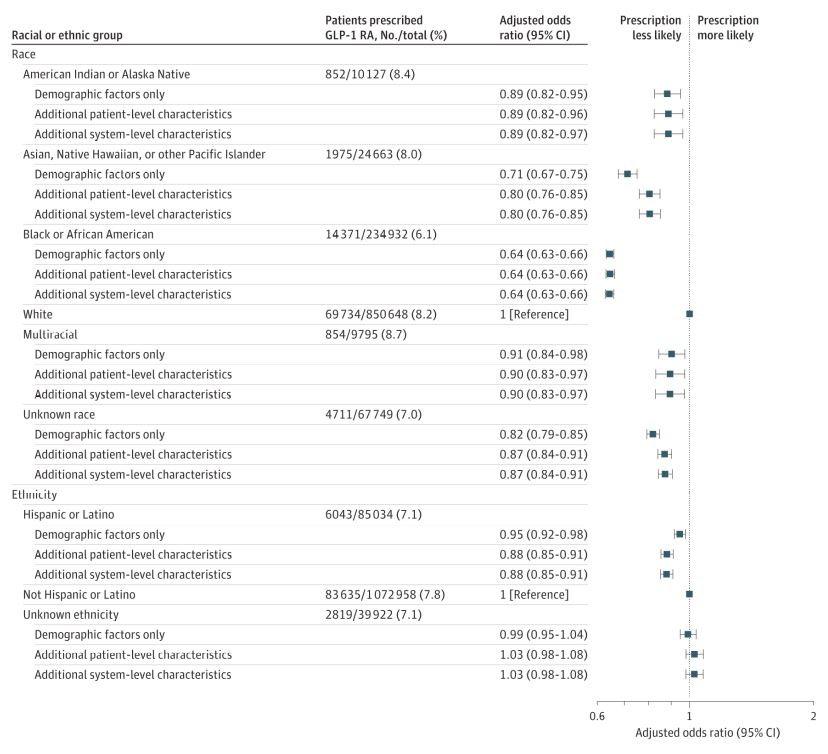
Click to Enlarge: The demographic factors only model includes age, sex, and self-identified race and ethnicity. The additional patient-level characteristics model includes demographic factors and zip code median income; zip code Social Deprivation Index; Veterans Health Administration (VHA) diabetes and service connection; rurality; smoking status; unhealthy alcohol use; hemoglobin A1C level; other antidiabetic agents; hypertension; body mass index; mental health diagnosis; atherosclerotic cardiovascular disease; heart failure; no chronic kidney disease; chronic kidney disease: estimated glomerular filtration rate and albuminuria categories; number of primary care, cardiology, endocrinology, and nephrology visits; VHA frailty index; and COVID-19 diagnosis. The additional system-level characteristics model includes VHA station parent facility-complexity level and US Census division. Source: JAMA Network
Prescription rates for SGLT2i and GLP-1 RA, respectively, were 11% and 7.1% among Hispanic or Latino patients and 10.7% and 7.8% among non-Hispanic or Latino patients.
“After accounting for patient- and system-level factors, all racial groups had significantly lower odds of SGLT2i and GLP-1 RA prescription compared with white patients. Black patients had the lowest odds of prescription compared with White patients (adjusted odds ratio, 0.72 [95% CI, 0.71-0.74] for SGLT2i and 0.64 [95% CI, 0.63-0.66] for GLP-1 RA),” study authors pointed out. “Patients of Hispanic or Latino ethnicity had significantly lower odds of prescription (0.90 [95% CI, 0.88-0.93] for SGLT2i and 0.88 [95% CI, 0.85-0.91] for GLP-1 RA) compared with non-Hispanic or Latino patients.”
The authors called for further research to better understand why those underlying prescribing differences exist and how they affect clinical outcomes.
Pharmacoequity at Issue
“Achieving pharmacoequity is central to overcoming health care disparities that persist across race and ethnic groups,” the study noted. “Racial and ethnic minority individuals have been less likely than white persons to be prescribed novel guideline-recommended therapies with proven effectiveness. These disparities may be particularly salient among patients with type 2 diabetes because Asian, Black, and Hispanic or Latino persons have a higher prevalence of diabetes and its complications than white patients.”
The authors emphasized that it is of public health importance to evaluate whether health care disparities exist in the prescription of guideline-recommended therapies that could reduce the cardiovascular and kidney complications of diabetes.
Background information in the study described how the availability SGLT2i and GLP-1 RA medications has altered how type 2 diabetes is managed, primarily because both classes have a positive effect on cardiovascular and kidney health. “Rather than relying on a glucose-centric approach to diabetes management and control, current guidelines recommend inclusion of these therapies to lower the risks of cardiovascular disease and chronic kidney disease (CKD) progression,” the researchers advised. “Recent research has shown that Black patients are less likely than white patients to be prescribed these therapies. However, prescription was strongly associated with income, which may have influenced the results given the high cost-sharing incurred by patients for these medications.”
The VHA, the largest integrated health system in the United States, provides uniform pharmacy access that offers discounted or free medications to patients, which minimizes the influence of medication costs.
The authors noted that their results are consistent with recent research that found low prescription rates of SGLT2i and GLP-1 RA among racial and ethnic minority groups in commercial and Medicare Advantage health plans. “Given the high cost-sharing for these medications, this study extends these findings to the VHA where the financial constraints impeding medication access are minimized”, they wrote.
In addition to the possible racial/ethnic inequities, the study raises questions about why the recommended drugs are so rarely prescribed in the VHA. “Consistent with these analyses and other recent research, the absolute rates of prescription in this study were low even for patients with concomitant atherosclerotic cardiovascular disease (ASCVD), heart failure, or CKD, the 3 conditions for which guidelines recommend SGLT2i and/or GLP-1 RA prescription irrespective of glycemic control,” the researchers pointed out, adding that their findings are in light with two recent VHA studies that found low prescription rates of GLP-1 RA among patients with established ASCVD and similar facility-level variability in SGLT2i and GLP-1 RA prescription.2,3
“The observed lower prescription of SGLT2i and GLP-1 RA for all race and ethnic groups relative to white patients and non-Hispanic patients persisted even after accounting for a broad array of patient- and system-level characteristics”, according to the authors. “Differences in comorbidities, social determinants of health at the zip code level, and access to primary and specialty care did not appear to explain observed racial and ethnic differences in these prescriptions. Indeed, system-level variation was low relative to overall variability in the prescription of SGLT2i and GLP-1 RA.”
Stating that racial and ethnic disparities in health and health care are pervasive in the United States, the authors advised, “Although to a smaller magnitude, these disparities have been reproduced in the VHA, indicating that financial constraints do not solely account for the observed differences across race and ethnic groups.”
They called for more analysis to determine if the issue is unrecognized racism or some other factor, such as the novelty of the medications.
- Lamprea-Montealegre JA, Madden E, Tummalapalli SL, et al. Association of Race and Ethnicity With Prescription of SGLT2 Inhibitors and GLP1 Receptor Agonists Among Patients With Type 2 Diabetes in the Veterans Health Administration System. JAMA. 2022;328(9):861–871. doi:10.1001/jama.2022.13885
- Mahtta D, Ramsey DJ, Lee MT, Chen L, et. al. Utilization Rates of SGLT2 Inhibitors and GLP-1 Receptor Agonists and Their Facility-Level Variation Among Patients With Atherosclerotic Cardiovascular Disease and Type 2 Diabetes: Insights From the Department of Veterans Affairs. Diabetes Care. 2022 Feb 1;45(2):372-380. doi: 10.2337/dc21-1815. PMID: 35015080; PMCID: PMC8914426.
- Al Rifai M, Vaughan EM, Abushamat LA, Lee M, et. al. Correlates of Glucagon-Like Peptide-1 Receptor Agonist Use Among Patients With Atherosclerotic Cardiovascular Disease and Type 2 Diabetes Mellitus (from the Department of Veterans Affairs). Am J Cardiol. 2022 Jun 1;172:7-10. doi: 10.1016/j.amjcard.2022.02.013. Epub 2022 Mar 17. PMID: 35305783.