COVID-19 Temporarily Raises Inpatient Prescribing Rates
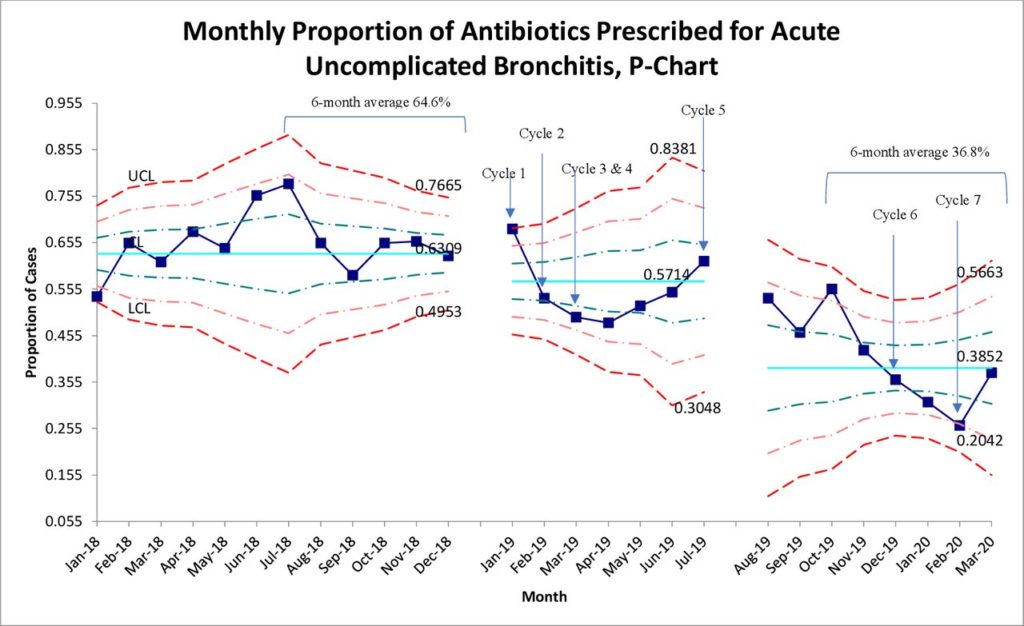
Click to Enlarge: SPC p-chart for monthly AUB/URI-NOS cases. *Χ2 comparison of the central limits of the three intervention periods had a p value=0.002. AUB, acute uncomplicated bronchitis; CL, control limit; LCL, lower control limit; NOS, not otherwise specified; SPC, Statistical Process Control; UCL, upper control limit; URI, upper respiratory tract infection.
PROVIDENCE, RI — VHA’s antibiotic stewardship programs implemented about eight years ago are beginning to pay off, but there is a lot of work left to do, according to new research.
A study presented recently at the European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) reported that outpatient antibiotic prescribing fell by almost 4% a year between 2011 and 2018. Because it is the largest integrated healthcare system in the United States, the VHA’s success likely had a significant effect on antibiotic trends nationwide, suggested the authors from the Providence, RI, VAMC.1
“We have seen positive steps taken to reduce antibiotic use in VA outpatient clinics, community-based outpatient clinics, emergency departments, and other outpatient settings, and healthcare teams should be congratulated for their ongoing work to reduce unnecessary antibiotic use,” explained lead author Haley Appaneal, PharmD, PhD.
“But over eight years, prescriptions for three of the most commonly prescribed outpatient antibiotics have changed little. And even with that drop in overall prescriptions, the threat of antibiotic resistance is increasing, so there is much more to be done.”
Background information in the presentation noted that, in 2014, VA mandated that its hospitals implement antibiotic stewardship programs, with significant decreases in inpatient antibiotic use since then. Researchers pointed out, however, that 80-90% of antibiotic use occurs in the outpatient setting, with at least 30% of outpatient antibiotics considered unnecessary.
That limited knowledge of trends in antibiotic utilization in VA outpatient settings is what led the authors, including participation from the Cleveland VAMC, the University of Rhode Island and Brown University, to assess trends in antibiotic use among VA outpatient clinics across the United States.
The study advised that the VA serves about 9.2 million veterans in more than 1,200 outpatient clinics and 140 hospitals. The authors assessed dispensed antibiotic prescriptions in the VA outpatient setting from 2011-2018 using VA pharmacy datasets.
Specifically, they calculated annual utilization in days of therapy (DOT) per 100 outpatient visits for all antibiotics and then separately for the five most common antibiotics:
- doxycycline,
- azithromycin,
- amoxicillin/clavulanate,
- amoxicillin,
- cephalexin
The team also included information on the most common fluoroquinolone, ciprofloxacin.
The study determined that, over eight years, several important trends occurred in outpatient antibiotic utilization, with the average annual percent decrease in all outpatient antibiotic use at 3.9% (95% CI -4.4 to -3.4%). That dropped from 39.6 DOT/100 visits in 2011 to 29.4 DOT/100 visits in 2018.
Researchers determined that the largest decline was in ciprofloxacin use, decreasing by 12.6% per year (95% CI -14.0 to -11.1%), followed by amoxicillin (AAPC -2.9%, 95% CI -3.4 to -2.5%) and cephalexin (AAPC -2.1%, 95% CI -2.6 to -1.7%).
On the other hand, utilization rates, as measured by total DOTs, were found to be highest for doxycycline, azithromycin and amoxicillin/clavulanate, with trends in their utilization being stable across the study period.
“Outpatient antibiotic prescribing has decreased in the national VA system, with an overall annual reduction of 3.9% and a reduction in ciprofloxacin use of 12.6% per year. This may be related to VA antibiotic stewardship programs. Despite reduced utilization of some antibiotics, use of the three most commonly prescribed outpatient antibiotics remained stable.”
“Our study identified target areas for outpatient antibiotic stewardship activities to reduce unnecessary antibiotic use in the USA. More than 2.8 million antibiotic-resistant infections occur every year, causing at least 35,000 deaths and $20 billion in health-care costs,” the authors wrote. “According to WHO, infections such as pneumonia, tuberculosis, sepsis, gonorrhea and foodborne diseases, are becoming harder, and sometimes impossible, to treat as antibiotics become less effective.”
VHA efforts to stem unnecessary antibiotic prescriptions have gone on for more than a decade, according to the report. In 2011, the National Antimicrobial Stewardship Task Force (ASTF) was established and, in 2014, the VHA required all of its hospitals to introduce antibiotic stewardship programs, driving down inpatient antibiotic use by 12% between 2008 and 2015.
A recent report noted, however, that inpatient antibiotic prescribing practices across the Veterans Health Administration (VA) experienced significant shifts during the coronavirus disease 2019 (COVID-19) pandemic. From 2015 to 2019, antibiotic use between January and May decreased from 638 to 602 days of therapy (DOT) per 1,000 days present (DP), while the corresponding months in 2020 saw antibiotic utilization rise to 628 DOT per 1,000 DP,” wrote UCLA and VA researchers in Infection Control and Hospital Epidemiology.2
The authors offered further explanation on the significant decrease in use of ciprofloxacin, pointing to the national trend away from fluoroquinolone prescriptions. Clinicians are urged to opt alternative agents because of the harms associated with use of that antibiotic class, including Clostridium difficile infection, adverse drug events and selection of resistance. The VA and the Food and Drug Administration both recommend limiting fluoroquinolone use for uncomplicated infections with safer treatment options, including acute sinusitis, acute bronchitis and uncomplicated urinary tract infections (UTI).
The study also noted that sulfamethoxazole/trimethoprim prescriptions, commonly used for UTIs, had a sharp decrease of about 7% a year.
The authors expressed concern about the continued widespread use from 2011 to 2018 of doxycycline, often used to treat skin infections and sexually transmitted infections; azithromycin, commonly used for chest, nose and throat infections; and amoxicillin/clavulanate, used for a range of infections, especially respiratory.
“Use of these three commonly prescribed antibiotics remains high and may be an appropriate target for antibiotic stewardship programs in the VA to further reduce inappropriate outpatient prescribing,” Appaneal said in a ECCMID press release. “It might also help combat resistance if national guidelines took stewardship principles into account when making disease-specific recommendations for antibiotic use.”
The study did not include prescriptions for patients filled outside the VA system, such as community pharmacies, and had more limited information on outpatient settings such as the emergency department or outpatient surgery.
Reductions for Bronchitis
Another recent report, from the Geriatric Research, Education and Clinical Center (GRECC at the VA Tennessee Valley Healthcare System in Nashville, provided an example of how reductions in antibiotic usage is being attached within the VHA Nashville Campus.
Those researchers pointed out that, while antibiotics are not recommended for treatment of acute uncomplicated bronchitis (AUB), they are prescribed 85% of the time within the VA system nationally.
The article in BMJ Open Quality reported on a quality improvement project designed to decrease antibiotic prescribing for AUB in community-based outpatient centers from 65% to <32% by April 2020.3
The authors described how, from January to December 2018, community-based outpatient clinics’ six-months average of prescribed antibiotics for AUB and upper respiratory infections was 63% (667 of 1,054) and 64.6% (314 of 486). After seven plan-do-study-act (PDSA) cycles were implemented by an interprofessional antimicrobial stewardship team between January 2019 and March 2020, the prescribing rate showed a sharp decline.
According to the study, balancing measures were a return patient phone call or visit within four weeks for the same complaint.
Results indicated that the AUB antibiotic prescribing rate decreased from 64.6% (314 of 486) in the six months prior to the intervention to 36.8% (154 of 418) in the final six months of the intervention. While no change was seen in balancing measures, the largest reduction in antibiotic prescribing occurred after implementation of PDSA 6 in which 14 high prescribers were identified and targeted for individualized reviews of when patients were prescribed antibiotics for AUB.
“Operational implementation of successful stewardship interventions is challenging and differs from the traditional implementation study environment,” the authors concluded. “As a nascent outpatient stewardship program with limited resources and no additional intervention funding, we successfully reduced antibiotic prescribing from 64.6% to 36.8%, a reduction of 43% from baseline. The most success was seen with targeted education of high prescribers.”
- Appaneal H, Caffey A, Liao X, Lopes V, et. al. National Trends in Outpatient Antibiotic Use in the United States (US): 2011 to 2018. Presented at European Congress of Clinical Microbiology & Infectious Diseases (ECCMID). Virtual. July 9-12,2021.
- Dieringer TD, Furukawa D, Graber CJ, Stevens VW, et. Al. Inpatient antibiotic utilization in the Veterans’ Health Administration during the coronavirus disease 2019 (COVID-19) pandemic. Infect Control Hosp Epidemiol. 2021 Jun;42(6):751-753. doi: 10.1017/ice.2020.1277. Epub 2020 Oct 20. PMID: 33077000; PMCID: PMC7653226.
- Johnson MC, Hulgan T, Cooke RG, Kleinpell R, Roumie C, Callaway-Lane C, Mitchell LD, Hathaway J, Dittus R, Staub M. Operationalising outpatient antimicrobial stewardship to reduce system-wide antibiotics for acute bronchitis. BMJ Open Qual. 2021 Jul;10(3):e001275. doi: 10.1136/bmjoq-2020-001275. PMID: 34210668.

