 SEATTLE — The most common risk factors worldwide for liver cancer are chronic infection with hepatitis B virus or hepatitis C virus, according to the American Cancer Society.
SEATTLE — The most common risk factors worldwide for liver cancer are chronic infection with hepatitis B virus or hepatitis C virus, according to the American Cancer Society.
Both of those infections lead to cirrhosis of the liver, but, in the United States, hepatitis C is the more common cause of HCC, while in Asia and developing countries, hepatitis B is more common, although patients infected with either of the viruses have a high risk of developing chronic hepatitis, cirrhosis and liver cancer. The risk is even higher if they are heavy drinkers, imbibing at least six alcoholic drinks a day, the ACS noted.
A new study pointed out that patients with chronic hepatitis B (CHB) infection routinely undergo screening for hepatocellular carcinoma (HCC), but it is not clear how beneficial the screening is.
A study team led by researchers from the VA Puget Sound Healthcare System and the University of Washington, both in Seattle, sought to evaluate the impact of screening with ultrasound and/or serum alpha-fetoprotein (AFP) on HCC-related mortality in patients with CHB.
To do that, researchers conducted a matched case-control study of patients with CHB receiving care through the VHA. Included were patients who died of HCC between Jan. 1, 2004, and Dec. 31, 2017, with controls being patients with CHB who did not die of HCC.
The study team matched cases to controls by CHB diagnosis date, age, sex, race/ethnicity, cirrhosis, antiviral therapy exposure, hepatitis B e antigen status and viral load. Researchers also identified screening ultrasound and AFPs obtained in the four years preceding HCC diagnosis in cases and the equivalent index date in controls.
Overall, 169 cases were matched to 169 controls.
With a lower likelihood of screening in cases corresponding to an association between screening and reduced risk of HCC-related mortality, the study found that fewer cases than controls underwent screening with either screening modality (33.7% vs. 58.6%) or both modalities (19.5% vs. 34.4%).
In multivariable conditional logistic regression, screening with either modality was associated with a lower risk of HCC-related mortality (adjusted odds ratio [aOR] 0.21, 95% CI 0.09-0.50), as was screening with both modalities (aOR of 0.13; 95% CI 0.04-0.43).
“HCC screening was associated with a substantial reduction in HCC-related mortality in VA patients with CHB,” the researchers concluded, pointing out that their findings demonstrated that liver cancer screening is associated with a reduction in the mortality from HCC in patients with hepatitis B infection.
The American Cancer Society pointed out that HBV and HCV both can spread from person to person via contaminated needle-sharing, unprotected sex or childbirth. While blood transfusions also can cause transmission, this remains rare in the United States, since blood products are tested for the viruses.
While HBV is more likely to cause symptoms, such as a flu-like illness and jaundice, most patients recover completely within a few months, and only a very small percentage of adults become chronic carriers, leading to a higher risk for liver cancer. The risk of developing a chronic condition is higher, however, in infants and small children who become infected, the ACS noted.
Conversely, HCV is less likely to cause symptoms but far more likely to lead to chronic infections, which can result in liver damage or even cancer. The cancer society advised that other viruses, such as the hepatitis A virus and hepatitis E virus, also can cause illness, but those patients do not develop chronic hepatitis or cirrhosis and do not have an increased risk of liver cancer.
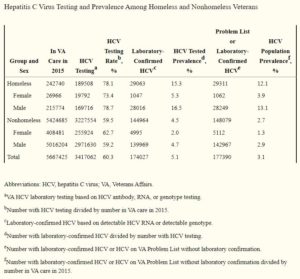
In veterans, HBV infection especially is concerned among those who suffer homelessness. Population prevalence for HBV was 0.99% (2395/242740) for homeless veterans and 0.40% (21611/5424685) among non-homeless veterans, according to a 2017 study in Clinical Infectious Diseases.2
“Among veterans, the HBV tested prevalence was 1.36%, while the population prevalence was 0.42%. In the homeless, 52.8% had been tested for HBV compared with 27.6% of the nonhomeless. Among those HBV tested, 2,306 homeless and 19,816 nonhomeless veterans had laboratory-confirmed HBV infection,” according to the report from the Providence, RI, VAMC. “Few homeless and nonhomeless veterans had HBV on their Problem List without laboratory confirmation (89 and 1795, respectively). The HBV tested prevalence among homeless and nonhomeless veterans was 1.80% and 1.32% respectively, and the population prevalence was 0.99% and 0.40%, respectively. The tested and population prevalence of HBV, in contrast to HIV and HCV, was only slightly higher among homeless males than among homeless females.”
- Su F, Weiss NS, Beste LA, Moon AM, Jin GY, Green P, Berry K, Ioannou GN. Screening is associated with a lower risk of hepatocellular carcinoma-related mortality in patients with chronic hepatitis B. J Hepatol. 2021 Apr;74(4):850-859. doi: 10.1016/j.jhep.2020.11.023. Epub 2020 Nov 24. PMID: 33245934; PMCID: PMC8045451.
- Noska AJ, Belperio PS, Loomis TP, O’Toole TP, Backus LI. Prevalence of Human Immunodeficiency Virus, Hepatitis C Virus, and Hepatitis B Virus Among Homeless and Nonhomeless United States Veterans. Clin Infect Dis. 2017 Jul 15;65(2):252-258. doi: 10.1093/cid/cix295. PMID: 28379316; PMCID: PMC6248754.

