USAMRIID Seeks Ways to Combat Novel Coronavirus Infection
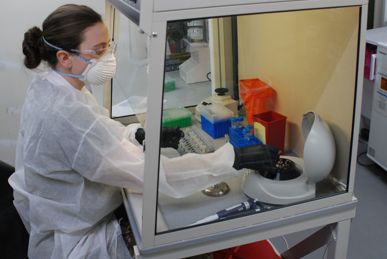
SPC Taylor Wolik, Medical Laboratory Specialist with the 1st Area Medical Laboratory, performs a diagnostic assay at the U.S. Army Medical Research Institute of Infectious Diseases field laboratory site at Fort Detrick, Md. USAMRIID provides specialized training to members of the 1st AML in conducting diagnostic assays to detect the presence of coronavirus and other biological agents in clinical or environmental samples.
Photo by William F Bill Discher, Medical Research and Development Command
FORT DETRICK, MD — As the novel coronavirus has continued to spread throughout the United States, infecting more than six million and killing more than 185,000 people, the U.S. Army has been on the front lines in an effort to protect the nation’s health and security.
It has done that by increasing understanding of the SARS-CoV-2 virus, using the specialized capabilities of the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick, MD.
On the therapeutic front, the institute partnered with researchers at the University of Illinois at Urbana-Champaign to advance research on a novel “decoy” receptor that could trick the SARS-CoV-2 virus and protect cells from attack. The Illinois team developed a receptor that mimics the angiotensin-converting enzyme 2 (ACE2) protein found on the surface of many types of cells, particularly those in the lungs, heart, arteries, kidneys and gastrointestinal system.1
Ordinarily, the ACE2 protein generates smaller proteins critical to functions such as blood pressure, blood volume and inflammation, but it also operates as a gateway for the SARS-CoV-2 virus to enter cells.
Erik Procko, PhD, professor of biophysics and quantitative biology at the University of Illinois at Urbana-Champaign, and colleagues analyzed ACE2 mutations and created a decoy enzyme that was designed to be more attractive as a receptor for the virus than the ACE2 enzyme. The virus binds strongly to the engineered, free-floating receptor, keeping the virus from attacking cells and preventing its spread.
The artificially optimized receptor may also have additional advantages, including combating some of the symptoms associated with the disease and limiting its ability to evade capture. “Administering a decoy based on ACE2 might not only neutralize infection, but also may have the additional benefit of rescuing lost ACE2 activity and directly treating aspects of COVID-19,” Procko said. “A benefit of a decoy receptor is that it closely resembles the natural receptor. Therefore, the virus cannot easily adapt to escape neutralization without simultaneously losing its ability to bind to its natural receptor. This means the virus has limited ability to acquire resistance.”
When Procko and his colleagues first posted their results, a colleague suggested connecting with Army researchers. “We were already in the process of testing several therapeutic candidates for SARS-CoV-2, and Erik’s approach seemed novel—and certainly compelling enough to give it a shot,” said Andrew Herbert, PhD, a senior research scientist at the Geneva Foundation, a non-profit that supports military medical research, who is based at USAMRIID.
Herbert and his colleagues determined the decoy was as effective a therapeutic as the best neutralizing antibodies currently available. They also found that it effectively bound to other coronaviruses that use ACE2 to enter cells, which have proven challenging for researchers up to this point.
Continue Reading this Article: Animal Model for COVID-19
