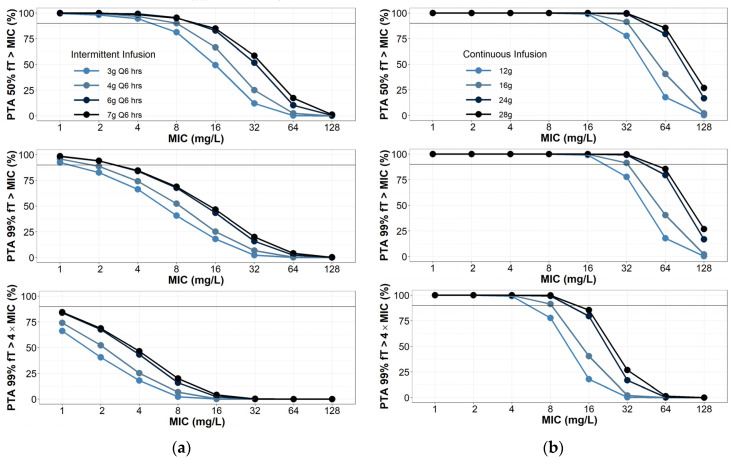
Click To Enlarge: Probability of target attainment for (a) piperacillin intermittent infusions; (b) continuous infusions. Intermittent infusions assumed to be infused over 30 min. Creatinine clearance was randomly selected between 100 and 130 mL/min, with 1000 virtual patients simulated per dosing group. Source: National Library of Medicine
BETHESDA, MD — Critical illness caused by burn and sepsis doesn’t alter how the body processes piperacillin and tazobactam (pip-tazo), an antibiotic and beta-lactamase inhibitor drug combination, according to the authors of a new study who suggest current guidelines for dosing are adequate.
The recent study published in the journal Antibiotics analyzed data from 19 critically ill patients (14 nonburn trauma and five burn) treated with pip-tazo in the MHS to determine how their bodies interacted with the administered drug, also known as pharmacokinetics. The pharmacokinetics of a given antibiotic may be affected when the body undergoes extreme changes, such as critical illness.i
The authors examined if there were any significant differences in the volume of distribution of antibiotics or creatinine clearance in burn versus nonburn trauma, critically ill patients. They also studied whether increased doses of pip-tazo would be required in burn patients after accounting for creatinine clearance, a way to estimate kidney function.
Two of the most important pathophysiologic changes common to many patients suffering from critical illness are increased leakiness of the capillaries and changes in kidney function, Daniel J. Selig, MD, first author of the study and deputy chief of Clinical Pharmacology and Experimental Therapeutics at the Center for Infectious Disease Research at Walter Reed Army Institute of Research, wrote in an email to U.S. Medicine.
When fluid leaks from capillaries into other body tissues, antibiotics may travel along with the fluid and increase the volume of the antibiotic that is contained by the body, which is known as the volume of distribution. Increased volume of distribution may lead to decreased antibiotic concentrations or accumulation of antibiotic in certain body tissues, sometimes requiring clinicians to increase the initial dose to overcome it, according to the study.
Also, the kidneys sometimes work overtime as a result of critical illness and clear antibiotics much more effectively, which is referred to as augmented renal clearance. Usually associated with very high creatinine clearances, augmented renal clearance can make it challenging to get enough antibiotics to patients to treat the infection, and higher doses or using alternative antibiotics are required, Selig explained.
This study found no significant differences in the volume of distribution or clearance of pip-tazo in burn and nonburn patients.
“Our research suggests that, for pip-tazo, current guidelines for dosing are adequate,” Selig explained. “However, critically ill patients from any cause may have unpredictable pharmacokinetics. Therefore, although studies like ours can help guide dosing decisions, the ultimate choice of pip-tazo dose must be decided by an expert in their respective field of critical care and should be supported by a multidisciplinary clinical team with expertise in that field.”
More Confident
“There is a notion that severe burn injury disrupts pharmacokinetics of antibiotics more than other causes of critical illness. Our research challenges this notion and allows clinicians to feel more confident when prescribing pip-tazo at doses recommended by society guidelines for common infections.”
The study suggests that, after accounting for creatinine clearance, doses would not need to be increased for burn patients compared to trauma patients based solely on pharmacokinetics. However, there is a high-reported incidence of augmented renal clearance in burn patients, and clinicians may choose higher doses based on pharmacodynamic (biochemical and physiological effects of drugs) factors. For critically ill patients with normal kidney function, continuous infusions of 13.5-18 grams of pip-tazo per day are preferred. If augmented renal clearance is suspected or the most stringent pharmacodynamic targets are desired, then continuous infusions of 31.5 grams of pip-tazo or higher may be required. This approach may be reasonable if therapeutic drug monitoring is used to ensure pip-tazo levels are not administered at levels greater than would be used in actual treatment, according to the study.
“From a pharmacokinetic perspective, critically ill patients, regardless of the cause of critical illness, don’t necessarily require increased doses of pip-tazo,” Selig said. “However, different causes of critical illness may be associated with different pharmacodynamic effects (i.e., decreased function of the immune system, different bacterial pathogens, etc.) that may lead a clinician to choose a higher or lower dose. Clinicians treating critically ill patients can generally feel confident using society guidelines for initial pip-tazo dosing decisions. However, dosing regimens should be tailored to their individual patients’ needs based off all available clinical data, their clinical expertise and resources available.”
When comparing the critical conditions of burn and sepsis, the study did not definitively determine which condition alters the pharmacokinetics of antibiotics more.
“Our research, along with literature review, suggests that there is no significant difference to the degree to which burn and sepsis alter pharmacokinetics of piperacillin and tazobactam (pip-tazo),” Selig wrote. “However, there is some suggestion from literature review that severe burn injury may alter pip-tazo pharmacokinetics more than sepsis. The main limitations to our study and most published studies reporting on pip-tazo pharmacokinetics in critically ill patients are relatively small sample sizes and lack of ideal comparison groups. It is important to remember that our study only looked at pip-tazo, and our findings may not be applicable to other antibiotics.”
In the future, it’s important to evaluate new and existing medications and medication combinations for pharmacokinetic variation from genetic differences, as well as altered physiologic conditions, he pointed out.
“Drug compounds only work well if they get to the target at the necessary concentration,” Selig said. “Scientists at Walter Reed Army Institute of Research are working to determine those reasons for the alteration and the necessary changes that are required to maximize efficacy and minimize risk.”
- Selig DJ, Akers KS, Chung KK, Kress AT, Livezey JR, Por ED, Pruskowski KA, DeLuca JP. Comparison of Piperacillin and Tazobactam Pharmacokinetics in Critically Ill Patients with Trauma or with Burn. Antibiotics (Basel). 2022 May 4;11(5):618. doi: 10.3390/antibiotics11050618. PMID: 35625262; PMCID: PMC9138153.

