PITTSBURGH—The VA’s success in reducing unnecessary antibiotic use in its hospitals has not trickled down to its outpatient clinics. That was underscored by a new study which determined that 76% of antibiotic prescriptions at primary care clinics in the Pittsburgh VA healthcare system were inappropriate prior to a recent educational intervention.
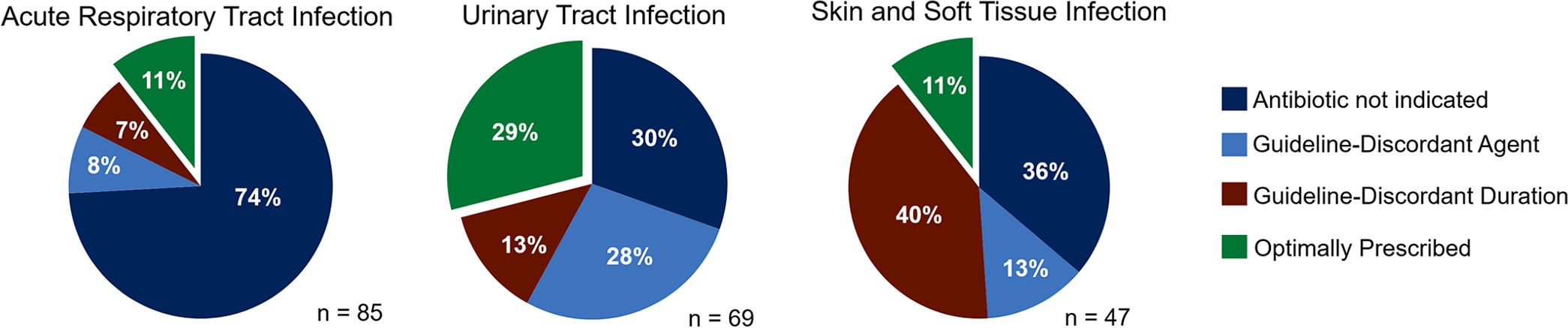
The study, published recently in Antimicrobial Agents and Chemotherapy, found that 49.7% of antibiotics prescriptions were unnecessary. In 12.3% of cases, an antibiotic was appropriate, but the wrong one was prescribed, based on national guidelines. In 14% of cases, the right antibiotic was prescribed, but the duration did not match guideline recommendations.1

“While we did not include other geographic regions or health systems in our study, I doubt that the Pittsburgh VA Healthcare System is an outlier for inappropriate antibiotic prescribing,” explained lead author Nathan Shively, MD, formerly of the Pittsburgh VA and now the medical director of the antimicrobial stewardship program at Allegheny Valley Hospital. “I think our findings are more likely to be a hint that prior studies might have underestimated the extent of the problem.”
Other studies of outpatient prescribing practices at the VA have identified high levels of antibiotic overprescribing, particularly for upper respiratory infections. Antibiotics provide no benefit for most acute respiratory infections, which are overwhelmingly viral, but they remain the leading reason for antibiotic prescriptions in outpatient settings at the VA and elsewhere. Instead, guidelines recommend symptomatic treatment for bronchitis, nonspecific upper respiratory infection, pharyngitis (unless a Group A streptococcus infection is confirmed), influenza and rhinosinusitis in most patients unless it persists for more than 10 days or worsens.3
Despite these long-standing recommendations, a study of prescribing patterns for acute respiratory infections in all emergency departments, as well as primary and urgent care clinics in the VA health system from 2005-2012 revealed a high—and rising—rate of antibiotic prescriptions.2 Over the eight years of the study, the percentage of acute respiratory infection diagnoses associated with an antibiotic prescription rose from 67.5% to 69.2%.
The researchers analyzed more than one million visits after excluding those that indicated the presence of comorbid conditions that increased the risk of bacterial infections or that represented a second visit for a respiratory infection within a month.
While the study was not structured to identify inappropriate prescriptions, the authors expected a “much lower overall proportion of antibiotic prescribing based on national treatment guidelines.” Notably, patients received antibiotics in more than 85% of sinusitis or bronchitis diagnoses.
The study also raised questions about the specific antibiotics selected. During the study period, the use of broad-spectrum antibiotics, particularly macrolides, increased from 36.8% to 47%, even though macrolides antibiotics are not first-line therapies for pharyngitis or sinusitis. “This trend is concerning given the lack of additional benefit of macrolides over narrow-spectrum antibiotics for ARI treatment; the increase in macrolide-resistant pneumococcal disease; and potential cardiotoxicity, especially considering the large number of veterans in our study who had cardiovascular comorbid conditions,” the authors said.
Broad-Spectrum Antibiotics Overused
Prescribing broad-spectrum antibiotics compounds the problems with resistance that providers seek to avoid, Shively told U.S. Medicine. “We’re in a difficult cycle in which knowledge of increasing bacterial resistance may prompt clinicians to utilize more broad spectrum antibiotics empirically, which then leads to more resistance.”
More recently, an analysis of prescribing behavior between March 2013 and February 2015 at the eight clinics in the outpatient primary care department at the Providence VAMC in Rhode Island determined that 38.4% of antibiotic prescriptions for respiratory infections were not warranted by the diagnosis.4 They found that providers in the nonteaching clinics had more than twice the rate of inappropriate prescribing for these indications than those in teaching clinics, 44% vs. 17.6%.
In the Pittsburgh study, almost three-quarters of antibiotic prescriptions written from September 2015 through August 2016 for acute respiratory tract infections were not indicated. While the study did not examine the reasons for inappropriate prescribing, Shively suggested that a lack of awareness of changes in guidelines and diminished effectiveness may account for some, adding that clinical uncertainty combined with pressure from patients and patient satisfaction scores also might contribute to the problem.
“Complicating this are patients who may have gotten used to receiving a Z-Pak every time they get a cold and come to the office requesting it. Part of our job is to educate providers which conditions are overwhelmingly likely to be viral in etiology and to help educate patients that antibiotics won’t help and might hurt,” he said.
Reducing Antibiotic Prescribing
Infectious disease specialists and other researchers in the VA have tested a variety of approaches to reduce inappropriate antibiotic prescriptions. The VA implemented a national antimicrobial stewardship initiative in 2014, which mandated the implementation of formal stewardship programs in all VAMCs.
Since its inception, “there has been a significant 12% percent decline in inpatient antibiotic use. Also during this period, VHA’s 30-day readmission and mortality rates decreased, intimating no untoward consequences of decreased antibiotic use,” said Gary Roselle, MD, the VA’s national program director for infectious disease.
Prescriptions for resistant gram-negative organisms, such as carbapenems, have declined as have rates of Clostridium difficile infection. The stewardship program include policies on antimicrobial use, extensive educational resources, public reporting of antibiotic use to NHSN, antibiogram development, provider feedback regarding prescribing practices and reporting that enables facilities to compare their antimicrobial use to other VA facilities of similar complexity, Roselle told U.S. Medicine.
Some of those approaches also might help bring down inappropriate prescribing in outpatient clinics. After documenting the baseline level of prescribing, the Pittsburgh researchers offered primary care providers education to share their data and discuss guidelines for antibiotic prescribing for the most-common conditions. Providers also received monthly comparisons showing their prescribing rate compared to their peers and a system target.
The program resulted in a 24.5% drop in antibiotic prescriptions overall in the first year. Inappropriate prescriptions for skin and soft-tissue infections were nearly eliminated, while those for urinary tract infections declined 40%. The rate of inappropriate prescribing for upper respiratory infections dropped, but not significantly.5 The use of guideline-discordant agents or durations did not change significantly.
Azithromycin prescriptions decreased 43.9%, and fluoroquinolone prescriptions declined 52%, but the use of both antibiotics continued to be inappropriate more than 70% of the time.
“Since then, the program has achieved marked and sustained reductions in antibiotic use,” Shively said. The results will be presented at ID Week in October and “will provide one model for how healthcare systems might improve their use of antibiotics.”
Faced with a similar problem, researchers from the VA Maryland Health Care System and the Salt Lake City VA Health System developed a clinical decision support system that flagged the use of fluoroquinolone and azithromycin for acute respiratory infections at the point of electronic prescription. The intervention reduced the proportion of unwarranted prescriptions of the two drugs from 22% to 3% over four years.6
The Miami VA Healthcare System has taken a different approach—educating patients on proper antibiotic use. The system’s website advises patients to take antibiotics as prescribed by a licensed healthcare professional and to recognize that antibiotics are not always necessary: “Antibiotics treat bacteria, not viruses. It is important that patients go to their provider knowing that an antibiotic prescription may not be the best solution. Let your provider make the call on whether an antibiotic prescription is right for you.”
Antimicrobial stewardship programs at the VA have implemented a number of initiatives that have shown success in reducing inappropriate antibiotic prescribing in hospitals and, increasingly, in outpatient settings.
The programs “can help educate clinicians and identify when it’s OK not to give antibiotics, help promote use of narrow spectrum antibiotics when appropriate and limit duration of therapy to help minimize the development of resistance,” said Shively. “There’s been increasing interest in the development of these programs and in research to identify best practices, but we still have a lot of work to do.”
1. Shively NR, Buehrle DJ, Clancy CJ, Decker BK. Prevalence of inappropriate antibiotic prescribing in primary care clinics within a Veterans Affairs health care system. Antimicrob Agents Chemother. 2018;62:e00337-18.
2. Jones BE, Sauer B, Jones MM, Campo J, Damal K, He T, Ying J, Greene T, Goetz MB, Neuhauser MM, Hicks LA, Samore MH. Variation in Outpatient Antibiotic Prescribing for Acute Respiratory Infections in the Veteran Population: A Cross-sectional Study. Ann Intern Med. 2015 Jul 21;163(2):73-80.
3. Harris AM, Hicks LA, Qaseem A, for the High Value Care Task Force of the American College of Physicians and for the Centers for Disease Control and Prevention. Appropriate Antibiotic Use for Acute Respiratory Tract Infection in Adults: Advice for High-Value Care From the American College of Physicians and the Centers for Disease Control and Prevention. Ann Intern Med. 2016;164:425–434.
4. Parente DM, Timbrook TT, Caffrey AR, LaPlante KL. Inappropriate prescribing in outpatient healthcare: an evaluation of respiratory infection visits among veterans in teaching versus non-teaching primary care clinics. Antimicrob Resist Infect Control. 2017 Mar 29;6:33.
5. Shively NR, Buehrle DJ, Clancy CJ, Decker BK. Reduction of overall and inappropriate antibiotic prescribing within a Veterans Affairs Primary Care System through Peer Comparison of Overall Antibiotic Prescribing Rates. Open Forum Infectious Diseases. October 2017;4(suppl_1):S275.
6. Rattinger GB, Mullins CD, Zuckerman IH, Onukwugha E, Walker LD, Gundlapalli A, et al. A Sustainable Strategy to Prevent Misuse of Antibiotics for Acute Respiratory Infections. PLoS ONE. 2012;7(12):e51147.

