
FORT DETRICK, MD — The Army’s Performance Triad promotes quality sleep, physical activity and good nutrition, but when sleep suffers, a new tool developed by the Army can help. An algorithm created by researchers at the Army Medical Research and Materiel Command in Fort. Detrick, MD, calculates precisely how much caffeine to consume and when to optimize alertness.
“We found that, by using our algorithm, which determines when and how much caffeine a subject should consume, we can improve alertness by up to 64%, while consuming the same total amount of caffeine,” explained senior author Jaques Reifman, PhD, a senior research scientist and director of DoD Biotechnology High Performance Computing Software Applications Institute and the Telemedicine and Advanced Technology Research Center at Fort. Detrick. “Alternatively, a subject can reduce caffeine consumption by up to 65% and still achieve equivalent improvements in alertness.”
The algorithm plugs in the user’s sleep-wake schedule and the maximum allowed caffeine, then produces the best caffeine-dosing strategy. The total maximum amount of caffeine permitted in the blood was limited to the level associated with a single 400 mg dose to prevent unsafe consumption. The tool builds on a previously validated model that predicts, based on the time of day, the degradation of performance on a psychomotor vigilance task caused by sleep loss and the boost in performance provided by caffeine.
The researchers calculated the optimum caffeine dose by comparing dosing strategies used in four earlier studies on sleep loss and then fine-tuning those to achieve better performance with the same amount of caffeine or the same performance with less caffeine.
“Our algorithm is the first quantitative tool that provides automated, customized guidance for safe and effective caffeine dosing to maximize alertness at the most needed times during any sleep-loss condition,” said Reifman. The research appeared in recently in the Journal of Sleep Research.1
The team plans to incorporate the algorithm into the 2B-Alert web tool and smartphone app it previously developed to “provide customized caffeine-consumption guidance to, for example, sustain the attention of sleep-deprived military personnel,” the authors said. Currently, the app learns how an individual responds to a lack of sleep and to caffeine and predicts their alertness but does not yet recommend quantities and timing of caffeine consumption to achieve peak performance.
Within the military setting, sleep deprivation remains a significant problem, despite efforts to increase sleep time available to servicemembers. The average servicemember sleeps about six hours per night, according to the Army Public Health Center, leaving them short an hour or two each day.

Force Readiness
That lack of sleep diminishes force readiness and can have a lasting impact on both active duty personnel and veterans. “In training and on the battlefield, inadequate sleep impairs essential abilities such as reaction times, the ability to detect and engage the enemy, and squad tactic coordination,” according to Army information on the Performance Triad. Sleep deficiency can also impair memory and concentration, contribute to errors and accidents, diminish decision-making quality, increase emotional lability and reduce awareness of functional impairment.
In the long-term, regularly getting less than seven hours of sleep contributes to weight gain, diabetes, hypertension, cardiovascular disease, depression, immune system disorders and increased risk of death, said sleep expert Raman K. Malhotra, MD, associate professor of neurology at the Washington University School of Medicine in St. Louis.
“These physiologic deficits cannot be overcome by motivation, initiative, or willpower—and can only be temporarily overcome by caffeine,” according to Army materials on sleep deprivation. But when caffeine is needed, getting the right amount at the right time matters.
Caffeine blocks adenosine receptors, which reduce feelings of sleepiness, and promotes alertness. Caffeine “can have a positive effect on your reaction times, mood and mental performance,” Malhotra told U.S. Medicine, but because it is short-acting “can require frequent doses throughout the day, as well as progressively higher doses to get the same effect, if you take it regularly.”
Consuming too much caffeine can cause diarrhea, sweating, nausea, increased heart and breathing rates and muscle tremors. Suddenly stopping caffeine can cause symptoms of withdrawal such as headaches, moodiness, sleepiness and reduced energy levels, Malhotra pointed out.
For the Army and other servicemembers, perhaps the most significant downside to consuming caffeine in high quantities or at the wrong time is its disruptive effect on sleep. Consuming caffeine even six hours before bedtime can reduce the total amount of sleep by a full hour, according to Malhotra, and reduce the amount of deep sleep during the night.
In addition, “caffeine can delay the timing of your body clock,” Malhotra noted. Previous research found that consumption of caffeine in the evening can cause a 40-minute shift in a person’s internal clock, lengthening the circadian rhythm and throwing off sleep schedules.2
High quantities can have a similar effect. The Army research team found in an earlier study that consuming high amounts of caffeine for several days along with short sleep cycles impairs individuals’ recovery when they are able to sleep.
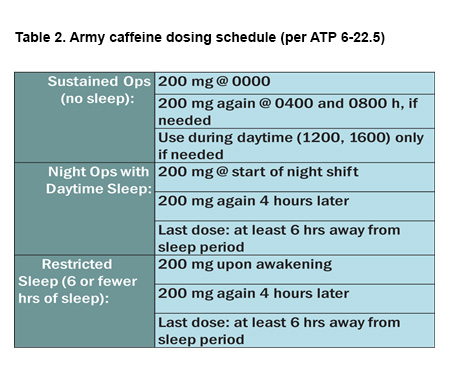
The Army’s currently recommended caffeine dosing schedule tries to minimize the impact on sleep by setting the last dose at least six hours before scheduled sleep.
The Fort Detrick team found that varying the amount of caffeine and the time it was consumed worked better than a consistent dose at the same time each day during a period of restricted sleep, such as the schedule currently recommended by the Army. Several changes optimized the benefit of caffeine, including delaying the first dose of caffeine on the first day and adding a dose later in the day for all but the last day of a restricted sleep schedule to compensate for significant impairment in the last two hours before scheduled sleep. Caffeine quantities also were backloaded to account for increased sleep pressure as the period of sleep deprivation grew.
The researchers noted that caffeine’s ability to counter impaired performance declines as sleep debt increases, with a significant reduction seen after four days with just five hours of sleep.
1Vital-Lopez FG, Ramakrishnan S, Doty TJ, Balkin TJ, Reifman J. Caffeine dosing strategies to optimize alertness during sleep loss. Journal of Sleep Research. 28 May 2018. Published online ahead of print.
2Burke TM, Markwald RR, McHill AW, Chinoy ED, Snider JA, Bessman SC, Jung CM, O’Neill JS, Wright KP Jr. Effects of caffeine on the human circadian clock in vivo and in vitro. Sci Transl Med. 2015 Sep 16;7(305):305ra146.

