By Jennifer Marquez
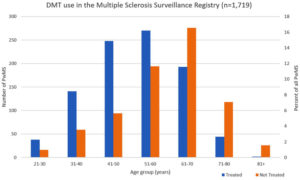
Current use of disease-modifying therapies (DMTs) in people with multiple sclerosis (PwMS) by age groups based on data from the US Department of Veterans Affairs (VA) Multiple Sclerosis Surveillance Registry (MSSR).
NEW YORK — Disease-modifying therapies (DMTs) help prevent permanent damage to the central nervous system when used early on to treat multiple sclerosis patients. Yet a recent study using VA data among others indicates that DMTs are under-prescribed among younger patients, even though they are most likely to receive the greatest benefit from treatment.1
Most people with MS, a neurological disorder that affects nearly one million U.S. adults, are diagnosed between the ages of 20 and 40. Research suggests, however, that the disease can cause significant damage to the brain and central nervous system years before clinical symptoms manifest. Initiating the use of DMTs as early as possible can help maximize brain health by reducing disease activity. In addition, relapses or flare-ups—periods when new symptoms appear or old symptoms become worse—tend to decrease with age. As a result, younger MS patients are also more likely to benefit from DMTs’ ability to lessen the frequency and severity of relapses.1
Despite the evidence demonstrating that these treatments are more valuable for younger patients who are relatively early in their disease progression, there has been a lack of data showing how DMTs are prescribed among different age populations. To learn more about prescribing patterns, a group of Icahn School of Medicine at Mount Sinai researchers collected demographic and clinical data from two large MS patient registries: The North American Research Committee on Multiple Sclerosis (NARCOMS) registry and the Multiple Sclerosis Surveillance Registry (MSSR), which was established by the U.S. Veterans Health Administration. They analyzed DMT use among more than 8,000 patients in two age groups: those 40 and under and those over 60.2
Researchers were from the VA Maryland Health Care System and Multiple Sclerosis Center of Excellence-East, both in Baltimore, MD, the VA North Texas Health Care System, the University of Alabama at Birmingham and Washington University School of Medicine in St. Louis.
Although DMT use was more prevalent among younger patients than older patients, the study team found that nearly one-third of MS patients under 40 were not being treated with DMTs, while more than one-third of patients older than 60 were still taking the drugs.
“DMTs for MS are more frequently used at younger ages when there is likely higher disease activity, yet a substantial proportion of younger persons with MS remain untreated,” the authors wrote in the study, which was published in Therapeutic Advances in Neurological Disorders. “As the probability of active disease declines with age and susceptibility to side effects increases, the risk versus benefit ratio of continuing DMTs in the elderly very likely diminishes.”
“It is now widely accepted that the earlier a person with MS is treated with an effective DMT, the better the long-term outcomes (e.g., fewer relapses, reduced disability, delayed disease progression),” said Bruce Bebo, executive vice president of research for the National MS Society. “It is critical that people with MS get on an effective disease modifying treatment as soon as possible. If the data reported in this paper is generalizable to the larger MS patient community, it is concerning to think that some young people are not receiving treatment.”
Why are DMTs underutilized in younger patient populations? One reason might be a lack of consistent access to affordable healthcare, which, the authors note, could explain the slightly higher rate of DMT use among U.S. veterans in the MSSR database compared to MS patients in the NARCOMS database, which reflects a more general population.
“The high cost of DMTs and insurance co-pays are often limiting factors that prevent patients with MS from starting and continuing DMTs,” said Mitchell Wallin, MD, one of the study’s authors, director of the VA’s Multiple Sclerosis Center of Excellence-East and professor of neurology at George Washington University School of Medicine and Health Sciences. “Lowering the financial toxicity of DMTs is critical for patients with MS. Providers should also encourage patients about the benefits of early therapy and find the DMT with the best fit (mode of delivery, side effects, efficacy).”
Drug Interactions
Other research has found that, as comorbidities rise, the likelihood of DMT use goes down. This might be because of concern about drug interactions or whether the treatment will be less beneficial to patients with other chronic health conditions. Additional reasons for not using DMTs could include side effects and a belief that the disease course will be mild.3
The researchers also discussed the downsides of DMT use among older patients. “With prolonged DMT use, there is an increased risk of adverse reactions especially in older persons with MS who are more susceptible to established side effects of DMTs, including infections and lymphopenia as well as multi-drug interactions,” they write. “In addition, disease activity in MS diminishes due to immune senescence, and relapses are less frequent in persons with MS over age 60 compared with those who are younger.”
The study authors question why providers continued to prescribe the drugs even as the risks increased and benefits decreased. They posited that providers might perceive that disease inactivity is due to treatment rather than the natural slowing of disease activity that comes with aging. Clinicians also are dealing with a lack of definitive evidence about the efficacy of DMTs among patients older than 55, who are usually excluded from clinical trials—something that needs to be addressed, according to the researchers.
“The safety of DMT use in the elderly remains unclear and deserves more rigorous study,” the authors wrote. “While recent retrospective data suggest relative safety in discontinuing DMTs in older patients without disease activity, these findings were not universal, and cases of disease worsening after stopping DMTs have been reported.”
“There is limited evidence of DMT efficacy in older adults, but many patients with MS are reluctant to stop their DMT as they age for fear of progression or new inflammatory activity,” Wallin told U.S. Medicine. “The ongoing DISCOMS trial is expected to address whether DMTs can be safely discontinued in stable MS patients over age 55. We need more data on the long-term impact of DMTs, especially in the elderly and in patients with co-morbid conditions such as cancer and chronic infections.”
Another recent study led by the Oklahoma City VAMC and the University of Oklahoma determined that veterans with MS who stuck to their DMT regimens had less decline in cognition, disease severity and disability related to MS, compared to groups that were less adherent or didn’t take their medications at all. That was the case after adjusting for age, gender, MS duration, and type, according to the report in the Journal of Central Nervous System Disease.4
The authors pointed out that it has been well understand that patients who adhere to their DMTs have lower rate of MS-related relapses and disability. What was unclear was whether adherence rate to DMTs had a meaningful effect on functional outcomes in veterans with MS.
To determine that, the researchers reviewed the electronic records of 279 veterans with MS who were periodically followed in their clinic. Patients were grouped according to their adherence to DMTs—either non-adherent, poorly adherent or adherent. The study team then looked at the effect on disability progression and time to sustained EDSS score of 6.
Most, 53%, of the MS patients were non-adherent to any DMT medication. Of the 47% who were taking medications at all, 42% had a good- and 5% had poor-adherence. For the patients reviewed, the mean age at MS onset was 36.6 and mean duration of MS for the sample was 24 years.
With mean initial EDSS and TFIM scores of 4.09 ± 2.9 SD and 104 ± 25.7 for the study sample, respectively, “The change in MMSE, TFIM scores, and time to sustained EDSS score of 6 significantly favored the good- compared to the non-adherence group,” according to the authors, who concluded, “Time to EDSS score of 6 was significantly prolonged in the good-adherence group.”
- Vladimiro Sinay, Manuel Perez Akly, Gisela Zanga, Celina Ciardi, Juan M Racosta. School performance as a marker of cognitive decline prior to diagnosis of multiple sclerosis. Multiple Sclerosis Journal. Published October 24, 2014. DOI: 10.1177/1352458514554054.
- Yinan Zhang, Amber Salter, Shan Jin, William J. Culpepper, II, Gary R. Cutter, Mitchell Wallin, Olaf Stuve. Disease-modifying therapy prescription patterns in people with multiple sclerosis by age. Therapeutic Advances in Neurological Disorders. Published March 31, 2021. DOI: 10.1177/17562864211006499.
- Tingting Zhang, Helen Tremlett, Stella Leung, Feng Zhu, Elaine Kingwell, John D Fisk, et al. Examining the effects of comorbidities on disease-modifying therapy use in multiple sclerosis. Neurology. Published April 5, 2016. DOI: 10.1212/WNL.0000000000002543.
- Rabadi MH, Just K, and Xu C. The impact of adherence to disease-modifying therapies on functional outcomes in veterans with multiple sclerosis. J Cent Nerv Syst Dis. Published online July 6, 2021. doi:10.1177/11795735211028769

