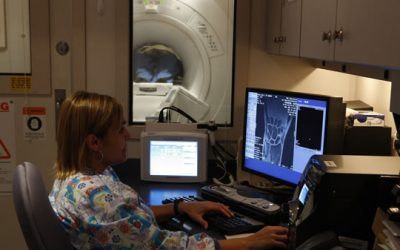
A new biomarker for multiple sclerosis might someday replace magnetic resonance imaging (MR)I, shown here at the Omaha, NE, VAMC. VA photo.
BALTIMORE—A University of Maryland research team has discovered a biomarker that can determine whether a patients has multiple sclerosis or is relapsing, thanks to VA funding. Now two VA organizations focused on technology transfer are working to bring the biomarker to market.
Approximately one million people in the United States have MS, among them about 60,000 veterans. In MS, the immune system attacks healthy tissue in the central nervous system and gradually destroys the myelin sheath that covers and protects the nerves.
Damage to the sheath disrupts electrical signaling between the brain and other parts of the body. That can cause a variety of symptoms, including: visual disruptions; muscle weakness; problems with gait, balance and coordination; numbness and pain; tremors; speech impediments; hearing loss; paralysis; and cognitive impairment.
Individuals with the most common form of the disease, relapsing-remitting multiple sclerosis, can go months or years between relapses. In patients with progressive multiple sclerosis, symptoms continue to worsen.
“Currently the diagnosis of the relapses is based on clinical findings (new symptoms which persists more than 24 hours) and by using brain or spine magnetic resonance imaging (MRI) to find active lesions which are also called gadolinium enhancing lesions,” said lead researcher Horea Rus, MD, PhD, professor of neurology at the University of Maryland.
Other tests used for diagnosis and disease monitoring include visual evoked potential testing and painful cerebrospinal fluid testing.
Brain MRIs are expensive and frequently require preapproval from insurance companies, delaying their use and the time to diagnosis or identification of a relapse. In addition, patients with claustrophobia require sedation for the exam and sometimes refuse to have an MRI at all, Rus explained.
Symptoms alone cannot reliably indicate either development of MS or a relapse, he noted, and patients who have no symptoms may still be experiencing disease progression. Even an MRI can fail to detect a relapse or progression in patients with “smoldering” MS, making a more reliable method important for monitoring disease progression and response to therapy.
Continue Reading:
