WASHINGTON—Researchers and policy makers estimated that 300,000 to 400,000 people in the U.S. had multiple sclerosis in 2010, but new data indicates that number grossly undercounted the number of people affected by the neurological disease.
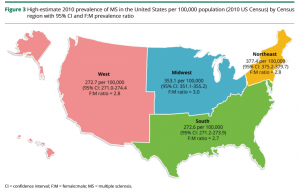
Surveillance data published in Neurology this spring indicates that that the actual numbers in 2010 were double the previous estimate. Using a new methodology, researchers at the VA and in the MS Prevalence Workgroup determined that about 727,000 individuals had MS at the beginning of the decade and that the number now approaches one million.1
How could so many people be missed?
Nationally, “we simply do not have a good surveillance network for neurological disease,” explained Mitchell Wallin, MD, MPH, director of the MS Center of Excellence-East, based in Washington, DC, and associate professor of neurology at George Washington University and the University of Maryland School of Medicine.
“We haven’t had a good prevalence study in 50 years,” Wallin told U.S. Medicine, and it turns out, “MS is more common than we thought.”
The study used data from the Optum, Truven Health and Kaiser Permanente Southern California datasets to model rates for privately insured individuals and the Centers for Medicare and Medicaid Services and VA healthcare databases for those covered by government-sponsored insurance programs. Altogether, the databases covered 45% of the U.S. population.
Based on previous studies, the researchers assumed a 5.0% rate of MS among individuals without insurance. The team then applied an algorithm previously validated against medical records in large datasets and healthcare systems to identify individuals with MS in the datasets. To capture cases missed because patients with relapsing disease might not see a healthcare provider during the period studied, the study adjusted for undercounting, as well.
Continue Reading: