Black Veterans Especially At Risk of AKI
S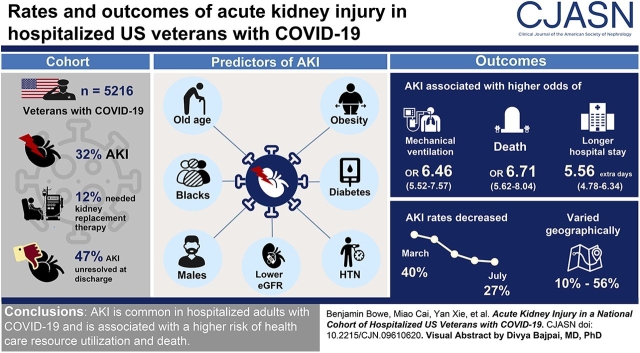 T. LOUIS — Nearly a third of veterans hospitalized with COVID-19 developed acute kidney injury, and half didn’t fully recover their kidney function by the time of hospital discharge, according to a new study.
T. LOUIS — Nearly a third of veterans hospitalized with COVID-19 developed acute kidney injury, and half didn’t fully recover their kidney function by the time of hospital discharge, according to a new study.
A report in the Clinical Journal of the American Society of Nephrology also indicated that AKI in veterans is associated with a higher risk of death and is disproportionately common in African Americans.1
VA Saint Louis Health Care System and Washington University-led researchers pointed out that past reports of COVID-19-associated AKI in the United States have been limited. To remedy that, the study team examined data from 5,216 VA patients hospitalized with COVID-19 FROM March to July.
“This is the first national study of AKI in COVID-19, and it told us that AKI is very common,” explained lead researcher Ziyad Al-Aly, MD. “It was also striking to see that nearly half of the veterans with AKI left the hospital with unresolved AKI—meaning that they will likely need long-term follow-up and care; they will also likely suffer long-term consequences lasting their lifetime. Their kidneys are scarred by COVID-19. Unresolved AKI and its long-term consequences are going to be part of the ‘long-haul COVID-19.’”
The study determined that 1,655 (32%) of the veterans had AKI: 58%, 13%, and 16% with Stage 1, 2 and 3 AKI, respectively, with 12% requiring kidney replacement therapy such as dialysis. Most, 80% of patients, developed AKI within one day of hospitalization, and 47% did not fully recover their kidney function by the time they were discharged.
Significant predictors of AKI development during COVID-19 hospitalization were older age, Black race, male gender, obesity, diabetes, hypertension and lower kidney function, according to researchers, who emphasized that the condition also was a predictor of worse overall outcomes. In fact, they said, AKI was associated with higher risks of requiring ventilation and longer hospital stays. It also was linked to a 6.7-times higher risk of death, according to the report.
“AKI was associated with higher mechanical ventilation use (odds ratio, 6.46; 95% confidence interval, 5.52 to 7.57) and longer hospital stay (5.56 additional days; 95% confidence interval, 4.78 to 6.34). AKI was also associated with higher risk of death (odds ratio, 6.71; 95% confidence interval, 5.62 to 8.04); this association was stronger in Blacks (P value of interaction <0.001),” the study noted.
The authors also advised that, because the association was stronger in Black veterans, that helped explain substantial geographic variability of AKI (ranging from 10% to 56%), with higher rates observed in regions with hospitals that cared for more Black veterans.
Between March and July 2020, AKI rates declined and proportions of AKI Stage 3 and AKI requiring kidney replacement therapy decreased,” the study found.
“AKI is common during hospitalization with COVID-19 and associated with higher risk of health care resource utilization and death,” the researchers concluded. “Nearly half of patients with AKI did not recover to baseline by discharge. Substantial geographic variation and temporal decline in rates and severity of AKI were observed.”
Minorities and COVID-19
A previous study of veterans found that non-Hispanic Black and Hispanic veterans were twice as likely as non-Hispanic white veterans to test positive for COVID-19 at the VA, even after accounting for other demographics, geographic location and underlying health conditions.2
The study published in the online journal PLOS Medicine reached those conclusions after reviewing records of about 5.8 million patients in the VA health system. It advised that, although no differences in 30-day mortality were observed among the groups, the disparities underscore the need to tailor COVID-19 prevention strategies to minority communites.1
VA Connecticut Healthcare System-led researchers focused on statistical associations between VA patients’ race/ethnicity and their detailed medical records, including COVID-19 testing records from Feb. 8 through July 22, 2020. Most of the participants, 91%, were male with 7% of Hispanic ethnicity, 19% Black and 74% white.
With more than 250,000 of the patients receiving a COVID-19 test during the study period, 16,317 tested positive, and 1,057 died within 30 days of testing. Researchers advise that Black and Hispanic veterans were more likely to receive a test and were more likely to test positive than white patients, even when accounting for other demographics underlying medical conditions and geographic location (Black vs. white adjusted odds ratio 1.93, 95% CI 1.85-2.01, p<0.001; Hispanic vs. white 1.84, 1.74-1.94, p<0.001).
- Bowe B, Cai M, Xie Y, Gibson AK, Maddukuri G, Al-Aly Z. Acute Kidney Injury in a National Cohort of Hospitalized US Veterans with COVID-19. Clin J Am Soc Nephrol. 2020 Nov 16:CJN.09610620. doi: 10.2215/CJN.09610620. Epub ahead of print. PMID: 33199414.2.
- Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, et. Al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLoS Med. 2020 Sep 22;17(9):e1003379. doi: 10.1371/journal.pmed.1003379. PMID: 32960880; PMCID: PMC7508372.

