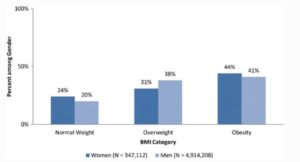
Click To Enlarge: The Obesity Epidemic in the Veterans Health Administration: Prevalence Among Key Populations of Women and Men Veterans. J GEN INTERN MED 32, 11–17 (2017). https://doi.org/10.1007/s11606-016-3962-1
IOWA CITY, IA — Nine years after their first introduction, direct acting oral anticoagulants (DOACs) hit the big time. When the American Heart Association/American College of Cardiology updated its guidelines for the management of non-valvular atrial fibrillation in 2019, they established DOACs as the preferred agents for anticoagulation, displacing warfarin after nearly 60 years as the only game in town.
DOACs offer greater predictability, standardized dosing, rapid onset of action, less interaction with food and other drugs, and limited need for monitoring compared to warfarin. The randomized clinical trials on which the approvals of apixaban, dabigatran, edoxaban, rivaroxaban, and betrixaban also showed better outcomes.
“Major randomized controlled trials showed that DOACs are as good or superior to warfarin in stroke prevention in patients with atrial fibrillation, and intracranial hemorrhage is lower with DOACs, while time in therapeutic range is higher,” Minang Turakhia, MD, MAS, director of cardiac electrophysiology at the VA Palo Alto Health Care System and executive director of the Center for Digital Health at Stanford University told U.S. Medicine.
Two years later, many patients remain on warfarin. One reason has been uncertainty about the use of the newer anticoagulants in obese patients. Studies showing the greater safety and efficacy of DOACs compared to warfarin had largely excluded individuals with body mass index above 35 kg/m2, a fact noted by the guidelines.
The weak evidence for use of DOACs in obese patients is particularly problematic. Obesity, defined as a BMI above 30 kg/m2, increases the risk of developing atrial fibrillation by 49% compared to non-obese individuals, with risk rising 5% to 7% with each unit increase in BMI. Obesity also raises the risk of progression from paroxysmal to persistent atrial fibrillation and elevates the risk of stroke, systemic embolism, death and disability. Additionally, the International Society of Hemostasis and Thrombosis recommends against using DOACs in patients with BMI greater than 40 kg/m2 or weight of 120 kg or more.
With 40% of American adults and a larger percentage of atrial fibrillation patients classified as obese, many clinicians had lingering concerns about the impact of the new anticoagulants’ pharmacokinetic and pharmacodynamic responses on dosing, patient management, and outcomes.
Reduced Hemorrhage
A study of more than 20,000 veterans published in Cardiovascular Drugs and Therapy in January should provide substantial reassurance. Researchers from the Iowa City, IA, VAMC, the University of Iowa College of Medicine, and National Kapodistrian University of Athens, Greece, found that the use of DOACs reduced the risk of hemorrhage, hemorrhagic stroke, and gastrointestinal bleeding in obese (weight of 120 kg or higher) and morbidly obese (BMI of 40 kg/m2) veterans compared to warfarin, while providing similar protection against ischemic stroke.1
The team analyzed outcomes for obese patients with atrial fibrillation treated in the VHA who initiated treatment between 2013 and 2018. The study included 6,052 patients on apixaban, 4,233 on dabigatran, 4,309 on rivaroxaban, and 13,417 on warfarin. Too few patients were prescribed edoxaban during the study period to include in the analysis. Patients had a mean age of 66.7 years; 91% were male and 80.4% were white.
With mean follow-up time to death or medication cessation was 19 months. During this time, the total study population experienced 211 total ischemic strokes and 837 major bleeding events.
Among all obese patients, dabigatran and rivaroxaban had lower rates of all-cause mortality than warfarin. Apixaban, on the other hand, had a higher risk of all-cause mortality. Dabigatran, rivaroxaban, and warfarin had comparable risk of ischemic stroke in this population, while apixaban’s risk was higher.
The researchers determined that the risk of major bleeding risk was clearly better among all the DOACs than warfarin for obese patients. Major bleeding risk and gastrointestinal bleeding were both significantly lower for patients receiving DOACs than those on warfarin. Apixaban, dabigatran, and rivaroxaban conferred markedly lower hemorrhagic stroke risk than warfarin in patients with BMI of 30 kg/m2 or higher.
Myocardial infarction rates were lower in obese patients taking dabigatran than the other DOACs or warfarin, which all had fairly similar rates. Across the board, the DOACs were associated with lower rates of heart failure admissions than warfarin in this patient group.
Within the subgroup of morbidly obese patients, with BMI of 40 kg/m2 or more, 3,414 were on apixaban, 2,405 on dabigatran, 2,340 on rivaroxaban, and 8,267 on warfarin. Among those with morbid obesity, all-cause mortality was lower with dabigatran than rivaroxaban. Apixaban had higher rates than both dabigatran and rivaroxaban.
No difference was noted in the risk of ischemic stroke or gastrointestinal bleeding between the DOACs in morbidly obese patients. Among the DOACs, apixaban and rivaroxaban had similar rates of major bleeding, with both higher than dabigatran. The risk of myocardial infarction in morbidly obese patients was highest in dabigatran and similar between apixaban and rivaroxaban.
Overall, morbidly obese patients followed the same pattern as the broader group of obese patients, with all DOACs having lower risk of all-cause mortality than warfarin, but comparable risk of stroke. All types of bleeding—major, gastrointestinal, and intracranial—were lower with all DOACs than warfarin.
The researchers noted that some of the differences in all-cause mortality rates among the DOACs could be attributable to heterogenous populations and differences in comorbidities. Other differences between the DOACs may be associated with differences in their mechanisms of action. Dabigatran is a direct thrombin inhibitor while apixaban and rivaroxaban are selective factor Xa inhibitors.
“Despite the effects of body weight extremes on pharmacologic properties of DOACs, our analysis suggests that the use of these agents is safe and effective in obese and morbidly obese patients compared with warfarin, with similar ischemic stroke risk but lower risk of bleeding, mortality, and heart failure,” the authors concluded.
- Briasoulis A, Mentias A, Mazur A, Alvarez P, Leira EC, Vaughan Sarrazin MS. Comparative Effectiveness and Safety of Direct Oral Anticoagulants in Obese Patients with Atrial Fibrillation. Cardiovasc Drugs Ther. 2021 Jan 6. doi: 10.1007/s10557-020-07126-2. Epub ahead of print. PMID: 33404923.
