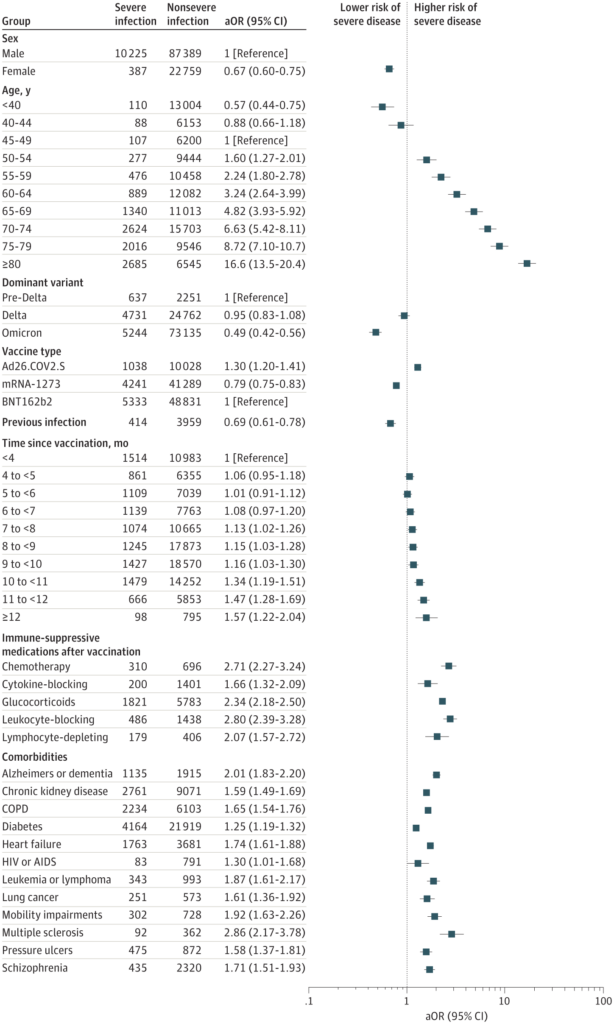
Click to Enlarge: All variables that met significance criteria (P < .05 after adjustment for multiple comparisons, and adjusted odds’ ratio [aOR] ≥1.50 or ≤0.67) and selected additional variables (eg, diabetes and HIV infection) chosen a priori for comparison. Source: JAMA Network Open
BOSTON — Although vaccination and boosting remain the best defense against COVID-19, breakthrough infections among those vaccinated and boosted are exceedingly common. For the majority of patients, these infections are relatively mild, but they can be severe for some, leading to hospitalizations for COVID-19 management and death.
Determining which patients are at greatest risk for severe disease despite vaccination can help inform efforts to promote booster vaccination and guide distribution of antiviral drugs for early treatment or pre-exposure prophylaxis, according to new research.
Identifying risk factors associated with severe disease was the primary aim of a nationwide retrospective cohort study of veterans who received a SARS-CoV-2 vaccination series and later developed laboratory-confirmed SARS-CoV-2 infection. The VA Boston Healthcare System-led study analyzed factors—including demographic characteristics, comorbidities, immunocompromised status and vaccination-related variables—associated with the development of severe versus nonsevere SARS-CoV-2 infection in vaccinated veterans treated at VA hospitals between Dec. 15, 2020, through Feb. 28, 2022.
Secondary aims were to identify and quantify risk factors in subgroups that may have different risk profiles (stratifying by immunocompromised status, age, sex and periods with delta or omicron variant predominance) and to evaluate whether associations with reductions in disease severity waned over time since the primary vaccination series and a single booster dose. The study was published in JAMA Network Open.1
Among 110,760 patients with infections following vaccination (97,614 [88.1%] men, mean [SD] age at vaccination, 60.8 [15.3] years; 26,953 [24.3%] Black, 11 259 [10.2%] Hispanic and 71,665 [64.7%] white). Also, 10 612 (9.6%) had severe COVID-19—defined as hospitalization within 14 days of a positive SARS-CoV-2 diagnostic test and either blood oxygen level of less than 94%, receipt of supplemental oxygen or dexamethasone, mechanical ventilation or death within 28 days. Association between severe disease and exposures was estimated using logistic regression models.
The most substantial association with risk of severe disease after vaccination was increasing age, the study found. Risk increased steadily among patients older than 50 such that patients aged 80 and older had an adjusted odds’ ratio of 16.58 (CI, 13.49-20.37) relative to patients aged 45 to 50 years.
Other key findings included:
- Risk of severe disease was reduced to a similar degree among vaccinated recipients who had also received booster vaccines and those with a history of COVID-19 infection before vaccination.
- Increasing time since initial vaccination appeared to be associated with severe outcomes in unstratified analyses; however, different effect estimates in the subcohorts suggested residual confounding.
- Risk of severe infection was lower during the period of omicron variant predominance than during the delta variant predominance period.
- An immunocompromised state—including that related to the receipt of immunosuppressive medications—was associated with increased risk of severe outcomes. The association was stronger if infection occurred after vaccination (i.e., producing an immunocompromised state at the time of exposure and subsequent infection) than if present only prior to vaccination, suggesting that “many patients receiving immunosuppressive medications at the time of vaccine develop durable protection, and the causal risk factor is immune status at the time of exposure,” the authors noted.
- The comorbidities most strongly associated with odds of severe disease include those identified early in the pandemic as the key risk factors for severe disease before vaccines were available. “Comorbidities indicating preexisting organ disease (eg, heart failure, chronic kidney disease, COPD, dementia) or a globally tenuous or frail state (eg, pressure ulcers, mobility impairments, low BMI) had stronger associations with risk than factors that contribute to future organ dysfunction (eg, hypertension),” the authors wrote.
- Risk was higher among the small number (890) of Native American individuals in the cohort—a finding the authors could not explain. However, they noted that “the similar risks among White, Black and African American, and Hispanic and Latino groups likely reflects the VA providing similar access in most regions.”
The authors said these findings could be used to bolster guidelines for administration of pre-exposure prophylaxis and to identify patients most likely to benefit from antiviral therapy. “Development of models to estimate the probability of a patient progressing to severe disease for individual risk assessment and to guide treatment and prophylaxis planning and outreach will require more sophisticated approaches, such as machine-learning models, to continue to inform best clinical practices for COVID-19 management,” they wrote.
- Vo AD, La J, Wu JT, Strymish JM, Ronan M, Brophy M, Do NV, Branch-Elliman W, Fillmore NR, Monach PA. Factors Associated With Severe COVID-19 Among Vaccinated Adults Treated in US Veterans Affairs Hospitals. JAMA Netw Open. 2022 Oct 3;5(10):e2240037. doi: 10.1001/jamanetworkopen.2022.40037. PMID: 36264571; PMCID: PMC9585432.
