WASHINGTON — MISSION Act critics have raised alarms about the legislation consolidating and expanding VA’s community care program– that healthcare provided by non-VA providers would fail to meet VA’s standards.
That concern, which President Joe Biden has said he will address, appears to be based in reality, according to a recent Government Accountability Office report; it urged VA to take immediate action to ensure community providers with a history of poor quality of care are excluded from its networks.
According to the report released last month, hundreds of providers removed from VA for providing poor care could still be part of its community care network, thanks to loopholes in the program’s screening.
In May 2019, VA began tracking providers that VA has found unfit to serve veterans in department facilities and making sure they could not participate in VA’s community care network. The tracking does not address providers removed from VA prior to that date, however.
VA’s screening resulted in the deactivation of 136 ineligible providers from participating in its Veterans Community Care Program (VCCP). Marking a provider as deactivated ensures that VA schedulers cannot schedule an appointment with that provider and that they cannot be added to the VCCP in the future.
In the investigation, GAO staff went back to July 2016 and found an additional 227 providers that have been removed from VA employment prior to May 2019 but who were still eligible to participate in the VCCP because they had been removed before the current screening process began.
According to the report, “VA stated it has no plans to further review these providers. VA officials said these providers were eligible to participate in the VCCP because they were removed from VA employment before the VA MISSION Act restrictions were effective.”
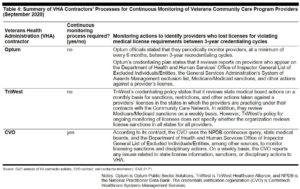
VA’s contracts with community care providers do not require the verification of the provider’s history of license sanctions, including a revoked license, in all states during credentialing. In addition, only one of the two VCCP contractors responsible for running the network has a process for verifying a provider’s licensing history. This is Optum, which currently is responsible for the VCCP in the eastern half of the continental United States, as well as Puerto Rico and the Virgin Islands. Still, neither contractor has a sufficient process for continually monitoring provider licenses, GAO investigators advised.
Monthly Audits
Monthly audits are one method VA has to ensure the quality of the providers in its current community care network. Every month, Office of Community Care officials select one out of every 2,000 providers in each of its network regions to review. The GAO examined these audits—2,405 from August 2019 to June 2020—and noted that VA had found 96 discrepancies.
Most were minor, involving things like a changed name. Auditors did discover some serious issues, however, that resulted in eight providers being removed from the network. Six were removed because of licensing issues, such as not having a current license and two for reasons involving not having an active Drug Enforcement Administration number.
GAO has investigated VA’s provider oversight in the past. In November 2017, it looked at a selection of VA facilities and found that VA officials rarely reported providers they had found problems with to the National Practitioner Data Bank (NPDB) or to state licensing boards. The result was that sometimes that provider went on to a non-VA facility or private practice where the same issues that caused them to be dismissed from VA continued.
VA did not take action to address this lack of reporting to state medical boards and the NPDB until December 2019.
“Our previous work and that of the VA Office of the Inspector General suggests the information contained in [the NPDB and state licensing boards] may not be complete and would not disqualify these former VA providers with quality of care concerns from participating in the VCCP,” GAO investigators wrote. “If providers with quality of care concerns participate in the VCCP, veterans will be at risk of being cared for by providers who have been removed from VA employment for failure to provide safe and appropriate care.”
GAO made three recommendations intended to shore up the VCCP’s credentialing process. The first is that VA should require its contractors to ensure that providers who had their medical license revoked in any state are excluded from the network. VA should also ensure that contractors develop a process for continuously monitoring eligibility requirements, such as using the National Practitioner Data Bank’s continuous query function, according to the report.
Lastly, VA should identify, analyze, and respond to any additional loopholes that might exist that would allow providers who have been removed from VA employment for providing unsafe care to serve veterans in the community.