OIG Said VA Needs to Do More About It
WASHINGTON, DC — VA should be doing more to identify and support victims of intimate partner violence (IPV), according to a recent VA Office of the Inspector General (OIG) report that also maintained that programs already in place are inconsistently implemented.
According to a 2018 study, 36% of women and 34% of men experience physical violence, sexual violence or stalking by an intimate partner in their lifetime. Those numbers go up for veterans and servicemembers, with some estimates reaching as high as 58%. Active duty servicemembers are three times more likely to perpetrate IPV than civilians.
The COVID-19 pandemic has resulted in a marked increase in IPV, with domestic violence calls increasing 8% during 2020. Researchers believe this is almost certainly an undercount, since most domestic violence incidents are not reported.
Not only has the pandemic exacerbated financial, occupational and home instability factors that are strongly linked with IPV, but it has caused people to remain trapped in a home with their abuser for long periods of time. Coupled with a reluctance to go to medical facilities for fear of contracting COVID-19, victims of IPV might have spent the last two years going undetected and unsupported.
In 2019, VA established an Intimate Violence Assistance Program (IPVAP) directive requiring a designated IPVAP coordinator at each facility to serve a subject-matter expert and consultant for IPV-related issues. It also required all facilities to “provide the full scope of services” when it came to IPV. That includes annual employee training, screening for IPV, coordination of support services and tracking and monitoring IPV referrals.
While the program is overseen nationally, facility directors are responsible for implementing local protocols, as well as the appointment of an IPVAP coordinator. However, according to the OIG report, more than half of the facilities do not have a local protocol in place.
“The absence of a local protocol may contribute to leader and staff confusion, and lack of knowledge about IPV roles, responsibilities, process, and procedures,” the investigators stated.
The weakness in facility protocol also might have contributed to inconsistent staff training around IPV. The majority of IPVAP coordinators surveyed by OIG reported providing training at fewer than half of new employee orientation sessions and to fewer than half of IPV screeners.
While VA requires all facilities to offer IPV screening and recommends screening all patients annually, it is not yet mandatory. Consequently, 14% of IPVAP coordinators reported that their facilities did not implement routine screening.
“To ensure robust monitoring and oversight, the OIG would expect use of the standardized instrument for routine screening nationally with identified benchmark metrics,” the OIG report stated.
VA also lacks metrics to measure the performance of the program as a whole. The OIG found that VA had not established any standardized program evaluation methods. Consequently, the IPVAP coordinators, who are responsible for program evaluation, had no measures by which to evaluate their facility.
VA leaders told investigators that, while performance metrics have not been prescribed, the data was being closely monitored and would soon be available in an online dashboard that will make evaluation easier.
There also was a wide discrepancy in how much time individual IPVAP coordinators dedicated to that role as compared to their other duties at the facility. While the majority reported that they spent over half of their time on IPVAP-related work, the coordinators serving the facilities with the most patients and the least patients reported spending less than 25% of their time on the role.
Half of IPVAP coordinators also reported being dissatisfied with support from IPVAP champions, who are positioned at the VISN level. VISN champions told investigators this was because they had no dedicated time for IPVAP activities and recommended that VA hire full-time staff to fill the VISN champion role.
During those interviews, VISN champions also recommended hiring dedicated IPVAP coordinators at facilities and implementing mandatory clinical reminders and screenings.
While the OIG did not go that far in their recommendations to VA, they did recommend that the department “determine the appropriate guidance for dedicated administrative staff support in consideration of the IPVAP coordinators’ responsibilities and take action as warranted.”
A study published this summer in the International Journal of Environmental Research and Public Health pointed out that intimate partner violence (IPV) is a major concern in military and veteran populations. The international researchers, including participation from the VA Boston Healthcare System, conducted an electronic search of PsycINFO, CINHAL, PubMed and the Cochrane Library databases to find studies that the prevalence of IPV perpetration or victimization reported by active duty (AD) military personnel or veterans.
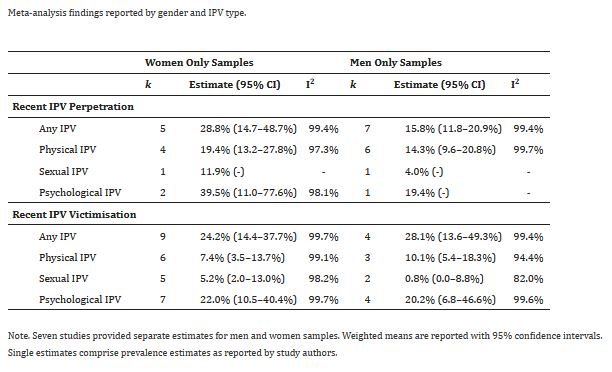
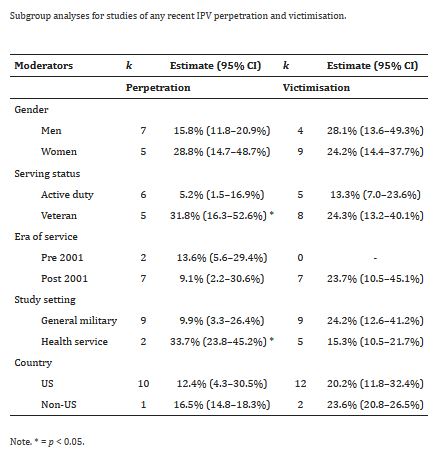
Ultimately, 31 studies involving 172,790 participants were included in meta-analyses. “These indicated around 13% of all AD personnel and veterans reported any recent IPV perpetration, and around 21% reported any recent victimization,” the authors reported. “There were higher rates of IPV perpetration in studies of veterans and health service settings, but no discernible differences were found according to gender, era of service, or country of origin.”
The study added that psychological IPV was the most common form identified, “while there were few studies of IPV impacts, or coercive and controlling behaviors.”
Researchers said their findings demonstrate that IPV perpetration and victimization occur commonly among military personnel and veterans and “highlight a strong need for responses across military and veteran-specific settings. However, there are gaps in understanding of impacts and context for IPV, including coercive and controlling behaviors, which are priority considerations for future research and policy”.1
- Cowlishaw S, Freijah I, Kartal D, Sbisa A, et. al. Intimate Partner Violence (IPV) in Military and Veteran Populations: A Systematic Review of Population-Based Surveys and Population Screening Studies. Int J Environ Res Public Health. 2022 Jul 21;19(14):8853. doi: 10.3390/ijerph19148853. PMID: 35886702; PMCID: PMC9316917.